Stem cell drugs: the next generation of pharmaceutical products
DOI:
https://doi.org/10.15419/bmrat.v3i10.128Keywords:
Stem cells, Stem cell drug, Pharmaceutical, Stem cell therapy, Stem Cell transplantation, hematopoietic stem cell, mesenchymal stem cell, HLA matchingAbstract
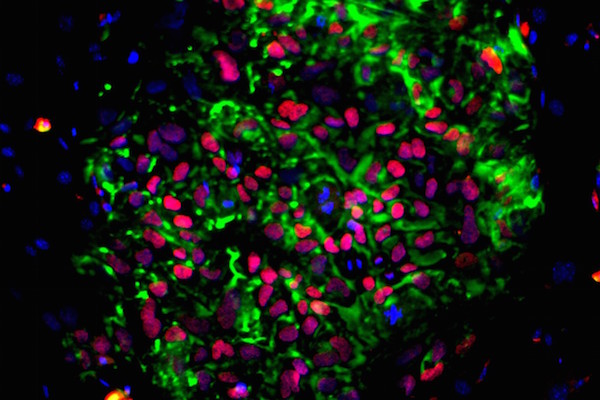
Stem cells represent a new treatment option in medicine and pharmacy. Stem cells have been increasingly used for the treatment of many diseases. In fact, they have spurred a new age of medicine called regenerative medicine. In recent years, regenerative medicine has become a new revolution in disease treatment, especially with the use of stem cell drugs. Stem cell drugs refer to live stem cell based products that used as drugs for particular diseases. Unlike autologous stem cell transplantation, stem cell drugs are “off-the-shelf” products that are ready to be used without requirement of any further manipulation. This review aims to summarize some of the approved stem cell drugs, and discuss the revolution of regenerative medicine and personalized medicine. As well, the review will discuss how stem cell drugs have led to a new direction in stem cell therapy, providing a new platform for patient needs.
References
2. Kotloff, R.M., V.N. Ahya, and S.W. Crawford, Pulmonary complications of solid organ and hematopoietic stem cell transplantation. American journal of respiratory and critical care medicine, 2004. 170(1): p. 22-48.
3. Tallman, M.S., et al., Conventional adjuvant chemotherapy with or without high-dose chemotherapy and autologous stem-cell transplantation in high-risk breast cancer. New England Journal of Medicine, 2003. 349(1): p. 17-26.
4. Lee, S.J., et al., High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood, 2007. 110(13): p. 4576-4583.
5. Petersdorf, E.W., et al., Optimizing outcome after unrelated marrow transplantation by comprehensive matching of HLA class I and II alleles in the donor and recipient. Blood, 1998. 92(10): p. 3515-3520.
6. Sasazuki, T., et al., Effect of matching of class I HLA alleles on clinical outcome after transplantation of hematopoietic stem cells from an unrelated donor. New England Journal of Medicine, 1998. 339(17): p. 1177-1185.
7. Dhot, P.S., et al., Cord blood stem cell banking and transplantation. Indian J Pediatr, 2003. 70(12): p. 989-92.
8. Armson, B.A., D.S. Allan, and R.F. Casper, Umbilical Cord Blood: Counselling, Collection, and Banking. J Obstet Gynaecol Can, 2015. 37(9): p. 832-46.
9. P De Miguel, M., et al., Immunosuppressive properties of mesenchymal stem cells: advances and applications. Current molecular medicine, 2012. 12(5): p. 574-591.
10. Hoogduijn, M.J., et al., The immunomodulatory properties of mesenchymal stem cells and their use for immunotherapy. International immunopharmacology, 2010. 10(12): p. 1496-1500.
11. Ankrum, J.A., J.F. Ong, and J.M. Karp, Mesenchymal stem cells: immune evasive, not immune privileged. Nature biotechnology, 2014. 32(3): p. 252-260.
12. Rasmusson, I., Immune modulation by mesenchymal stem cells. Experimental cell research, 2006. 312(12): p. 2169-2179.
13. Karussis, D., et al., Safety and immunological effects of mesenchymal stem cell transplantation in patients with multiple sclerosis and amyotrophic lateral sclerosis. Archives of neurology, 2010. 67(10): p. 1187-1194.
14. Lalu, M.M., et al., Safe ty of Cell Therapy with Mesenchymal Stromal Cells (SafeCell): A Systematic Review and Meta-Analysis of Clinical Trials. PloS one, 2012. 7(10): p. e47559.
15. Hare, J.M., et al., A randomized, double-blind, placebo-controlled, dose-escalation study of intravenous adult human mesenchymal stem cells (prochymal) after acute myocardial infarction. Journal of the American College of Cardiology, 2009. 54(24): p. 2277-2286.
16. Wang, Y., et al., Safety of mesenchymal stem cells for clinical application. Stem cells international, 2012. 2012.
17. Takahashi, K. and S. Yamanaka, Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. cell, 2006. 126(4): p. 663-676.
18. Till, J.E. and C.E. Mc, A direct measurement of the radiation sensitivity of normal mouse bone marrow cells. Radiat Res, 1961. 14: p. 213-22.
19. Dominici, M., et al., Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy, 2006. 8(4): p. 315-317.
20. Ren, G., et al., Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell stem cell, 2008. 2(2): p. 141-150.
21. Majumdar, M.K., et al., Human marrow-derived mesenchymal stem cells (MSCs) express hematopoietic cytokines and support long-term hematopoiesis when differentiated toward stromal and osteogenic lineages. Journal of hematotherapy & stem cell research, 2000. 9(6): p. 841-848.
22. Caplan, A.I. and J.E. Dennis, Mesenchymal stem cells as trophic mediators. Journal of cellular biochemistry, 2006. 98(5): p. 1076-1084.
23. Chen, L., et al., Paracrine factors of mesenchymal stem cells recruit macrophages and endothelial lineage cells and enhance wound healing. PloS one, 2008. 3(4): p. e1886.
24. Hocking, A.M. and N.S. Gibran, Mesenchymal stem cells: paracrine signaling and differentiation during cutaneous wound repair. Experimental cell research, 2010. 316(14): p. 2213-2219.
25. Bai, L., et al., Human bone marrow‐derived mesenchymal stem cells induce Th2‐polarized immune response and promote endogenous repair in animal models of multiple sclerosis. Glia, 2009. 57(11): p. 1192-1203.
26. Mello, D.B., et al., Adipose Tissue-Derived Mesenchymal Stromal Cells Protect Mice Infected with Trypanosoma cruzi from Cardiac Damage through Modulation of Anti-parasite Immunity. PLoS Negl Trop Dis, 2015. 9(8): p. e0003945.
27. Barcia, R.N., et al., What Makes Umbilical Cord Tissue-Derived Mesenchymal Stromal Cells Superior Immunomodulators When Compared to Bone Marrow Derived Mesenchymal Stromal Cells? Stem Cells Int, 2015. 2015: p. 583984.
28. Cutler, A.J., et al., Umbilical cord-derived mesenchymal stromal cells modulate monocyte function to suppress T cell proliferation. J Immunol, 2010. 185(11): p. 6617-23.
29. Prasanna, S.J., et al., Pro-inflammatory cytokines, IFNgamma and TNFalpha, influence immune properties of human bone marrow and Wharton jelly mesenchymal stem cells differentially. PLoS One, 2010. 5(2): p. e9016.
30. Weiss, M.L., et al., Immune properties of human umbilical cord Wharton's jelly-derived cells. Stem Cells, 2008. 26(11): p. 2865-74.
31. Hu, L., et al., Exosomes derived from human adipose mensenchymal stem cells accelerates cutaneous wound healing via optimizing the characteristics of fibroblasts. Sci Rep, 2016. 6: p. 32993.
32. Burrello, J., et al., Stem Cell-Derived Extracellular Vesicles and Immune-Modulation. Front Cell Dev Biol, 2016. 4: p. 83.
33. Lai, R.C., et al., Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. Stem Cell Res, 2010. 4(3): p. 214-22.
34. Bian, S., et al., Extracellular vesicles derived from human bone marrow mesenchymal stem cells promote angiogenesis in a rat myocardial infarction model. J Mol Med (Berl), 2014. 92(4): p. 387-97.
35. Feng, Y., et al., Ischemic preconditioning potentiates the protective effect of stem cells through secretion of exosomes by targeting Mecp2 via miR-22. PLoS One, 2014. 9(2): p. e88685.
36. Arslan, F., et al., Mesenchymal stem cell-derived exosomes increase ATP levels, decrease oxidative stress and activate PI3K/Akt pathway to enhance myocardial viability and prevent adverse remodeling after myocardial ischemia/reperfusion injury. Stem Cell Res, 2013. 10(3): p. 301-12.
37. Zhang, Z., et al., Pretreatment of Cardiac Stem Cells With Exosomes Derived From Mesenchymal Stem Cells Enhances Myocardial Repair. J Am Heart Assoc, 2016. 5(1).
38. Zhou, Y., et al., Exosomes released by human umbilical cord mesenchymal stem cells protect against cisplatin-induced renal oxidative stress and apoptosis in vivo and in vitro. Stem Cell Res Ther, 2013. 4(2): p. 34.
39. Jiang, Z.Z., et al., Exosomes secreted by human urine-derived stem cells could prevent kidney complications from type I diabetes in rats. Stem Cell Res Ther, 2016. 7: p. 24.
40. Li, T., et al., Exosomes derived from human umbilical cord mesenchymal stem cells alleviate liver fibrosis. Stem Cells Dev, 2013. 22(6): p. 845-54.
41. Hyun, J., et al., MicroRNA125b-mediated Hedgehog signaling influences liver regeneration by chorionic plate-derived mesenchymal stem cells. Sci Rep, 2015. 5: p. 14135.
42. Narayanan, R., C.C. Huang, and S. Ravindran, Hijacking the Cellular Mail: Exosome Mediated Differentiation of Mesenchymal Stem Cells. Stem Cells Int, 2016. 2016: p. 3808674.
43. Nakamura, Y., et al., Mesenchymal-stem-cell-derived exosomes accelerate skeletal muscle regeneration. FEBS Lett, 2015. 589(11): p. 1257-65.
44. Zhang, Y., et al., Effect of exosomes derived from multipluripotent mesenchymal stromal cells on functional recovery and neurovascular plasticity in rats after traumatic brain injury. J Neurosurg, 2015. 122(4): p. 856-67.
45. Kim, D.K., et al., Chromatographically isolated CD63+CD81+ extracellular vesicles from mesenchymal stromal cells rescue cognitive impairments after TBI. Proc Natl Acad Sci U S A, 2016. 113(1): p. 170-5.
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.