Autologous osteochondral transplantation for treatment of cartilage defects in osteoarthritic knee: preliminary results
DOI:
https://doi.org/10.15419/bmrat.v3i11.138Abstract
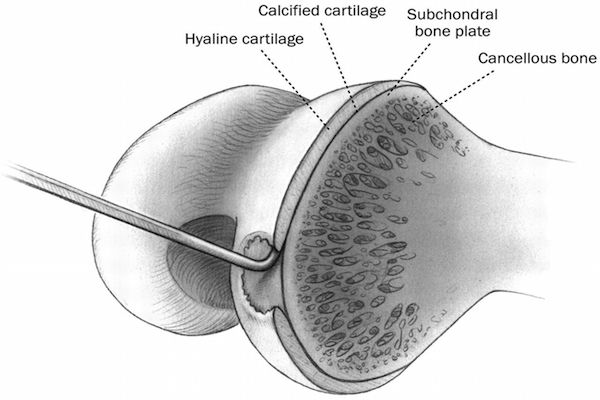
Introduction: Osteoarthritis is a contributing factor for pain and loss of function of the knee. Osteoarthritis results in many damages to the knee; one of the most common damages that is difficult to recover is cartilage injury. This study aims to apply autologous osteochondral transplantation (OAT) under knee arthroscopy for the treatment of knee cartilage defects.
Methods: This was a prospective, descriptive and non-controlled study. Patients were diagnosed as having osteoarthritis, as confirmed by 1cm2 – 3cm2 cartilage defects. Arthroscopic OAT was performed on each patient. Treatment efficacy and safety were evaluated based on Lysholm, Oxford Knee Scores (OKS) and pain scales (VAS) after 3, 6, 12 and 18 months.
Results: From 3/2014 - 8/2016, 61 cases (54 women and 7 men) participated in the study. The average age was 55 ± 8 years old. Most cases had cartilage defects in the medial condyle. Results showed that Lysholm, OKS scores and VAS scales improved after 12 months of treatment. Of the cases, 33 of 61 were followed out to 18 months; these patients showed improvement in knee function and pain scores. There was 1 case with incomplete matching between the plug and receiving site and 1 case with a broken plug. At the final stage of monitoring, there were no patients who experienced complications, such as broken instruments or fracture of condyle, nor who experienced early postoperative complications, such as infection and bleeding.
Conclusion: Autologous osteochondral transplantation via arthroscopy is a safe and promising method for the treatment of knee cartilage defects in patients with average osteoarthritis.
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
