Artemisinin-induced delayed hemolysis after administration of artesunate and artesunate-amodiaquine in malaria-free Wistar rats
DOI:
https://doi.org/10.15419/bmrat.v4i4.160Keywords:
Antimalarial, Artemisinin, Delayed hemolysis, Drug-induced hemolysisAbstract
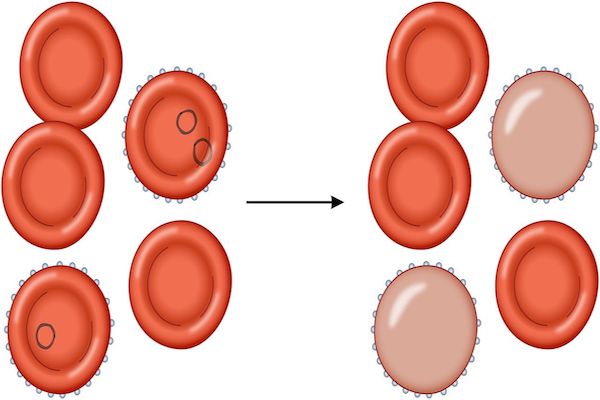
Background: Hemolysis is common in malaria infection and during the course of treatment. Previous studies have reported delayed post-artemisinin hemolysis occurring in naïve and immune individuals treated with parenteral or oral artemisinin-derivatives. This study aims to understand if delayed hemolysis occurs in the absence of malaria parasites and the underlying mechanisms for the hemolytic effects after administration of two antimalarial drugs to malaria-free Wistar rats. Methods: Forty animals were randomized into 5 groups of eight animals each; they received 4 mg/kg artesunate for 7 days (AS), 4 mg/kg artesunate plus 10mg/kg amodiaquine for 3 days (ASQ), 10mg/kg amodiaquine for 3 days (AQ), distilled water [normal control], (Control) and 1mg/kg phenylhydrazine for 1 day to induce hemolysis (PHZ) groups respectively. Packed cell volume (PCV), white blood cell differential count and serum haptoglobin (Hpt) levels were determined in all groups on day 4 and 18 to detect hemolysis. Mean values were compared using t-test and ANOVA with p values <0.05 taken to be significantly different. Results: Post-treatment mean PCV on day 4 was significantly lower than day 18 in all groups except AS group which had similar PCV all through evaluation. Although AQ had lowest mean PCV on day 4, by day 18, mean PCV returned to normal and hpt levels was significantly higher than AS and ASQ groups (p<0.001). Hpt level (mean ± sem) for AS, ASQ, AQ, and control on day 18 were: 18.67 ± 0.004, 50.66 ± 0.014, 73.06 ± 0.003, and 74.13 ± 0.032 mg/dl respectively (p < 0.0001). On day 18, AS and ASQ had significantly lower Hpt level compared to day 4 (p <0.001). No neutropenia was observed during the study. Conclusion: Artesunate induces delayed hemolysis in malaria-free animals possibly through an oxidative toxic effect on the red blood cell membrane. Delayed post-treatment hemolysis was not observed with artesunate-amodiaquine or amodiaquine alone.
References
Anaba, F.C., Ahiante, B.O., and Pepple, D.J. (2012). In vitro hemolytic effect of sulfadoxine/pyrimethamine and artemether/lumefantrine on malaria parasitized erythrocytes of female patients. Pak J Pharm Sci 25, 851-855.
Angus, B.J., Chotivanich, K., Udomsangpetch, R., and White, N.J. (1997). In vivo removal of malaria parasites from red blood cells without their destruction in acute falciparum malaria. Blood 90, 2037-2040.
Arguin, P.M. (2014). Case definition: postartemisinin delayed hemolysis. Blood 124, 157-158.
Bethell, D., Se, Y., Lon, C., Socheat, D., Saunders, D., Teja-Isavadharm, P., Khemawoot, P., Darapiseth, S., Lin, J., and Sriwichai, S. (2010). Dose-dependent risk of neutropenia after 7-day courses of artesunate monotherapy in Cambodian patients with acute Plasmodium falciparum malaria. Clinical Infectious Diseases 51, e105-e114.
Beutler, E., Duparc, S., and Group, G.P.D.W. (2007). Glucose-6-phosphate dehydrogenase deficiency and antimalarial drug development. The American journal of tropical medicine and hygiene 77, 779-789.
Boillat, O., Spechbach, H., Chalandon, Y., and Eperon, G.A. (2015). Post-artesunate delayed haemolysis‒report of four cases and review of the literature. Swiss medical weekly 145, w14181.
Chavada, R., Hui, S.H., O'Connor, S., Akima, S., and Gosbell, I. (2015). Post-artesunate delayed haemolysis in severe imported Plasmodium falciparum malaria. The Medical journal of Australia 203, 364-364.
Chikezie, P.C. (2014). Comparative erythrocyte glutathione S-transferase activity profile of Non-malarious guinea pigs (cavia tschudii) administered pyrimethamine/sulfadoxine and artemether/lumefantrine combination therapies. Thrita 3.
Chotivanich, K., Udomsangpetch, R., Dondorp, A., Williams, T., Angus, B., Simpson, J., Pukrittayakamee, S., Looareesuwan, S., Newbold, C., and White, N. (2000). The mechanisms of parasite clearance after antimalarial treatment of Plasmodium falciparum malaria. Journal of Infectious Diseases 182, 629-633.
Clark, I., Rockett, K., and Cowden, W. (1991). Proposed link between cytokines, nitric oxide and human cerebral malaria. Parasitology Today 7, 205-207.
Clark, R.L. (2014). Hypothesized cause of delayed hemolysis associated with intravenous artesunate. Medical hypotheses 82, 167-170.
Conran, N. (2014). Intravascular hemolysis: a disease mechanism not to be ignored. Acta haematologica 132, 97-99.
Control, C.f.D., and Prevention (2013). Published reports of delayed hemolytic anemia after treatment with artesunate for severe malaria--worldwide, 2010-2012. MMWR Morbidity and mortality weekly report 62, 5.
Cooke, B.M., Mohandas, N., and Coppel, R.L. (2004). Malaria and the red blood cell membrane. Paper presented at: Seminars in hematology (Elsevier).
Dondorp, A.M., Pongponratn, E., and White, N.J. (2004). Reduced microcirculatory flow in severe falciparum malaria: pathophysiology and electron-microscopic pathology. Acta tropica 89, 309-317.
Finaurini, S., Ronzoni, L., Colancecco, A., Cattaneo, A., Cappellini, M.D., Ward, S.A., and Taramelli, D. (2010). Selective toxicity of dihydroartemisinin on human CD34+ erythroid cell differentiation. Toxicology 276, 128-134.
Garba, I., and Ubom, G. (2005). Total serum lactate dehydrogenase activity in acute Plasmodium falciparum malaria infection. Singapore medical journal 46, 632.
Gbotosho, G.O., Okuboyejo, T., Happi, C.T., and Sowunmi, A. (2014). Fall in Hematocrit per 1000 Parasites Cleared From Peripheral Blood: A Simple Method for Estimating Drug-Related Fall in Hematocrit After Treatment of Malaria Infections. American journal of therapeutics 21, 193-197.
Gu, H., Warhurst, D.C., and Peters, W. (1986). Hemolysis induced by artemisinin and its derivatives in vitro. Zhongguo yao li xue bao= Acta pharmacologica Sinica 7, 269.
Howes, R.E., Piel, F.B., Patil, A.P., Nyangiri, O.A., Gething, P.W., Dewi, M., Hogg, M.M., Battle, K.E., Padilla, C.D., and Baird, J.K. (2012). G6PD deficiency prevalence and estimates of affected populations in malaria endemic countries: a geostatistical model-based map. PLoS Med 9, e1001339.
Jauréguiberry, S., Ndour, P.A., Roussel, C., Ader, F., Safeukui, I., Nguyen, M., Biligui, S., Ciceron, L., Mouri, O., and Kendjo, E. (2014). Postartesunate delayed hemolysis is a predictable event related to the lifesaving effect of artemisinins. Blood 124, 167-175.
Jeney, V., Balla, J., Yachie, A., Varga, Z., Vercellotti, G.M., Eaton, J.W., and Balla, G. (2002). Pro-oxidant and cytotoxic effects of circulating heme. Blood 100, 879-887.
Jollow, D.J., and McMillan, D.C. (2001). Oxidative stress, glucose-6-phosphate dehydrogenase and the red cell. In Biological Reactive Intermediates VI (Springer), pp. 595-605.
Krishna, S., Uhlemann, A.-C., and Haynes, R.K. (2004). Artemisinins: mechanisms of action and potential for resistance. Drug Resistance Updates 7, 233-244.
Kurth, F., Lingscheid, T., Steiner, F., Stegemann, M.S., Bélard, S., Menner, N., Pongratz, P., Kim, J., von Bernuth, H., and Mayer, B. (2016). Hemolysis after Oral Artemisinin Combination Therapy for Uncomplicated Plasmodium falciparum Malaria. Emerging Infectious Diseases 22, 1381.
Lee, J., Krajden, S., Graham, C., Boggild, A.K., Pavenski, K., Keystone, J.S., and Kain, K.C. (2015). Severe delayed hemolysis associated with regulated parenteral antimalarial drug. Emerging infectious diseases 21, 164.
Meshnick, S., Tsang, T., Lin, F., Pan, H., Chang, C., Kuypers, F., Chiu, D., and Lubin, B. (1989). Activated oxygen mediates the antimalarial activity of qinghaosu. Progress in clinical and biological research 313, 95-104.
Meshnick, S.R., Yang, Y., Lima, V., Kuypers, F., Kamchonwongpaisan, S., and Yuthavong, Y. (1993). Iron-dependent free radical generation from the antimalarial agent artemisinin (qinghaosu). Antimicrobial Agents and Chemotherapy 37, 1108-1114.
Molta, N., Oguche, S., Pam, S., Omalu, I., Afolabi, B., Odujoko, J., Amajoh, C., Adeniji, B., Wuyep, V., and Ekanem, O. (2003). Amodiaquine treatment of uncomplicated malaria in children, in an area of chloroquine-resistant Plasmodium falciparum in north-central Nigeria. Annals of Tropical Medicine & Parasitology 97, 663-669.
Muhia, D., Thomas, C., Ward, S., Edwards, G., Mberu, E., and Watkins, W. (1994). Ferriprotoporphyrin catalysed decomposition of artemether: analytical and pharmacological implications. Biochemical pharmacology 48, 889-895.
Newton, P.N., Chotivanich, K., Chierakul, W., Ruangveerayuth, R., Teerapong, P., Silamut, K., Looareesuwan, S., and White, N.J. (2001). A comparison of the in vivo kinetics of Plasmodium falciparum ring–infected erythrocyte surface antigen–positive and–negative erythrocytes. Blood 98, 450-457.
Ngole, S.I.U., Theresa, N.-A., Moses, S., Thomas, N., Manka, N.E., and Titanji, V. (2010). Haematological changes and recovery associated with treated and untreated Plasmodium falciparum infection in children in the Mount Cameroon Region. Journal of Clinical Medicine and Research 2, 143-151.
Nuchsongsin, F., Chotivanich, K., Charunwatthana, P., Fausta, O.-S., Taramelli, D., Day, N.P., White, N.J., and Dondorp, A.M. (2007). Effects of malaria heme products on red blood cell deformability. The American journal of tropical medicine and hygiene 77, 617-622.
Olliaro, P.L., and Mussano, P. (2003). Amodiaquine for treating malaria. The Cochrane Library.
Omotuyi, I.O., Nwangwu, S. C., Okugbo, O. T., Okoye, O. T., Ojieh, G. C., and Wogu, D. M. (2008). Hepatotoxic and hemolytic effects of acute exposure of rats to artesunate overdose. African Journal of Biochemistry Research 2, 107-110.
Orjih, A.U. (1996). Haemolysis of Plasmodium falciparum trophozoite‐infected erythrocytes after artemisinin exposure. British journal of haematology 92, 324-328.
Park, Y., Diez-Silva, M., Popescu, G., Lykotrafitis, G., Choi, W., Feld, M.S., and Suresh, S. (2008). Refractive index maps and membrane dynamics of human red blood cells parasitized by Plasmodium falciparum. Proceedings of the National Academy of Sciences 105, 13730-13735.
Pasvol, G., Clough, B., and Carlsson, J. (1992). Malaria and the red cell membrane. Blood reviews 6, 183-192.
Price, R.N., Simpson, J.A., Nosten, F., Luxemburger, C., Hkirjaroen, L., ter Kuile, F., Chongsuphajaisiddhi, T., and White, N.J. (2001). Factors contributing to anemia after uncomplicated falciparum malaria. The American journal of tropical medicine and hygiene 65, 614-622.
Raffray, L., Receveur, M.-C., Beguet, M., Lauroua, P., Pistone, T., and Malvy, D. (2014). Severe delayed autoimmune haemolytic anaemia following artesunate administration in severe malaria: a case report. Malaria journal 13, 398.
Rehman, K., Lötsch, F., Kremsner, P.G., and Ramharter, M. (2014). Haemolysis associated with the treatment of malaria with artemisinin derivatives: a systematic review of current evidence. International Journal of Infectious Diseases 29, 268-273.
Roederer, M.W., McLeod, H., and Juliano, J.J. (2011). Can pharmacogenomics improve malaria drug policy? Bulletin of the World Health Organization 89, 838-845.
Rolling, T., Agbenyega, T., Krishna, S., Kremsner, P.G., and Cramer, J.P. (2015). Delayed haemolysis after artesunate treatment of severe malaria–Review of the literature and perspective. Travel medicine and infectious disease 13, 143-149.
Scott, M.D., Meshnick, S.R., Williams, R.A., Chiu, D.T., Pan, H.C., Lubin, B.H., and Kuypers, F.A. (1989). Qinghaosu-mediated oxidation in normal and abnormal erythrocytes. The Journal of laboratory and clinical medicine 114, 401-406.
Sinclair, D., Donegan, S., Isba, R., and Lalloo, D.G. (2012). Artesunate versus quinine for treating severe malaria. Cochrane Database Syst Rev 6.
Sowunmi, A., Gbotosho, G.O., Happi, C., Okuboyejo, T., Folarin, O., Balogun, S., and Michael, O. (2009). Therapeutic efficacy and effects of artesunate-mefloquine and mefloquine alone on malaria-associated anemia in children with uncomplicated Plasmodium falciparum malaria in southwest Nigeria. The American journal of tropical medicine and hygiene 81, 979-986.
Tangnitipong, S., Thaptimthong, T., Srihirun, S., Unchern, S., Kittikool, D., Udomsangpetch, R., and Sibmooh, N. (2012). Extracellular heme enhances the antimalarial activity of artemisinin. Biological and Pharmaceutical Bulletin 35, 29-33.
Van Malderen, C., Van Geertruyden, J.-P., Machevo, S., González, R., Bassat, Q., Talisuna, A., Yeka, A., Nabasumba, C., Piola, P., and Daniel, A. (2012). Glucose-6-phosphate dehydrogenase deficiency, chlorproguanil-dapsone with artesunate and post-treatment haemolysis in African children treated for uncomplicated malaria. Malaria journal 11, 139.
Vickers, A.E., Sinclair, J.R., Fisher, R.L., Morris, S.R., and Way, W. (2010). Blood cell oxidative stress precedes hemolysis in whole blood–liver slice co-cultures of rat, dog, and human tissues. Toxicology and applied pharmacology 244, 354-365.
Wang, J.X., Tang, W., Shi, L.P., Wan, J., Zhou, R., Ni, J., Fu, Y.F., Yang, Y.F., Li, Y., and Zuo, J.P. (2007). Investigation of the immunosuppressive activity of artemether on T‐cell activation and proliferation. British journal of pharmacology 150, 652-661.
WHO (2013). World Health Organization (2013). WHO Information Note on Delayed Haemolytic Anaemia following Treatment with Artesunate. WHO/GMP Information Note, October 2, 2013.
Yang, Z.S., Zhou, W.L., Sui, Y., Wang, J.X., Wu, J.M., Zhou, Y., Zhang, Y., He, P.L., Han, J.Y., Tang, W., et al. (2005). Synthesis and immunosuppressive activity of new artemisinin derivatives. 1. [12(beta or alpha)-Dihydroartemisininoxy]phen(ox)yl aliphatic acids and esters. Journal of medicinal chemistry 48, 4608-4617.
Yeo, T.W., Lampah, D.A., Tjitra, E., Gitawati, R., Kenangalem, E., Piera, K., Granger, D.L., Lopansri, B.K., Weinberg, J.B., and Price, R.N. (2009). Relationship of cell-free hemoglobin to impaired endothelial nitric oxide bioavailability and perfusion in severe falciparum malaria. Journal of Infectious Diseases 200, 1522-1529.
Zhou, W.L., Wu, J.M., Wu, Q.L., Wang, J.X., Zhou, Y., Zhou, R., He, P.L., Li, X.Y., Yang, Y.F., Zhang, Y., et al. (2005). A novel artemisinin derivative, 3-(12-beta-artemisininoxy) phenoxyl succinic acid (SM735), mediates immunosuppressive effects in vitro and in vivo. Acta pharmacologica Sinica 26, 1352-1358.
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
