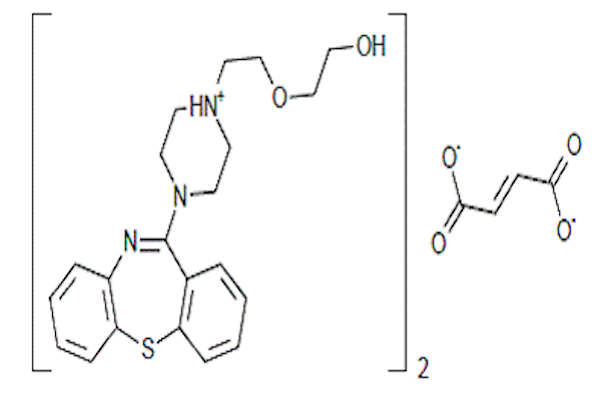
Evaluation of Quetiapine Fumarate and its Solid Lipid Nanoparticles as antipsychotic drug in rat model of schizophrenia
DOI:
https://doi.org/10.15419/bmrat.v4i08.203Keywords:
Biology, Antipsychotic drugs, Catecholamines, Excitatory and inhibitory amino acids, Nanoparticles, Schizophrenia, MedicineAbstract
Background: The present study compares the efficacy of quetiapine fumarate (QF) and QF-loaded solid lipid nanoparticles (QFSLN) as antipsychotic drugs for schizophrenia.
Methods: To induce schizophrenia-like symptoms, a group of rats was injected intraperitoneally (i.p.) with ketamine (25mg/kg b.w.) for 1 week to establish a rat model of schizophrenia. The incidence of schizophrenic symptoms was estimated to be equivalent to the control group. To estimate the pronounced antipsychotic effect of QF, a low dose (LD) of 10 mg/kg b.w. and a high dose (HD) of 30 mg /kg b.w. were orally administrated to two groups of rats (designated L.QF and H.QF) for 3 weeks (2 weeks without ketamine injection; the last week with ketamine). To achieve the optimal therapeutic response of QF drug, 2 other groups of rats were administered orally the equivalent low and high doses of QF in its solid lipid nanoparticle form (L.QFSLN) and (H.QFSLN) for 3 weeks in the same manner. The treatments were given after 1 h of ketamine injection. To assess the effect of different doses of treatment on hyperlocomotion and cognitive impairment induced by ketamine, an open field test and passive avoidance test were conducted. In addition, excitatory and inhibitory amino acids, as well as catecholamines, were estimated in brain regions (cortex and hippocampus). The study was extended to estimate the side effects of different treatments on hepatorenal functions and lipid profile. Additionally, samples were subjected to immunohistochemical analysis.
Results: QFSLN treatment showed enhanced effect over QF in a dose-dependent manner with minimal side effects in schizophrenic rats. In addition, immunohistochemical examinations of brain tissues confirmed the biochemical data.
References
<li class="show">Adams, J.M., and Cory, S. (2001). Life-or-death decisions by the Bcl-2 protein family. Trends in biochemical sciences 26, 61-66. <a href="https://doi.org/10.1016/S0968-0004(00)01740-0 ">https://doi.org/10.1016/S0968-0004(00)01740-0 </a></li>
<li class="show">Arion, D., Unger, T., Lewis, D.A., Levitt, P., and Mirnics, K. (2007). Molecular evidence for increased expression of genes related to immune and chaperone function in the prefrontal cortex in schizophrenia. Biological psychiatry 62, 711-721. <a href="https://doi.org/10.1016/j.biopsych.2006.12.021">https://doi.org/10.1016/j.biopsych.2006.12.021 </a></li>
<li class="show">Armitage, P.B., G and Matthews, JNS (2008). Comparison of several groups. In Statistical methods in medical research (Oxford: Blackwell Science Ltd), pp. 208-235.</li>
<li class="show">Barch, D.M., Carter, C.S., Braver, T.S., Sabb, F.W., MacDonald, A., Noll, D.C., and Cohen, J.D. (2001). Selective deficits in prefrontal cortex function in medication-naive patients with schizophrenia. Archives of general psychiatry 58, 280-288. <a href="https://doi.org/10.1001/archpsyc.58.3.280">https://doi.org/10.1001/archpsyc.58.3.280</a></li>
<li class="show">Bellino, S., Paradiso, E., and Bogetto, F. (2006). Efficacy and tolerability of quetiapine in the treatment of borderline personality disorder: A pilot study. The Journal of clinical psychiatry 67, 1042-1046. <a href="https://doi.org/10.4088/JCP.v67n0705">https://doi.org/10.4088/JCP.v67n0705 </a></li>
<li class="show">Blasi, P., Schoubben, A., Traina, G., Manfroni, G., Barberini, L., Alberti, P.F., Cirotto, C., and Ricci, M. (2013). Lipid nanoparticles for brain targeting III. Long-term stability and in vivo toxicity. International journal of pharmaceutics 454, 316-323. <a href="https://doi.org/10.1016/j.ijpharm.2013.06.037">https://doi.org/10.1016/j.ijpharm.2013.06.037</a></li>
<li class="show">De Oliveira, L., Fraga, D.B., De Luca, R.D., Canever, L., Ghedim, F.V., Matos, M.P.P., Streck, E.L., Quevedo, J., and Zugno, A.I. (2011). Behavioral changes and mitochondrial dysfunction in a rat model of schizophrenia induced by ketamine. Metabolic brain disease 26, 69-77. <a href="https://doi.org/10.1007/s11011-011-9234-1">https://doi.org/10.1007/s11011-011-9234-1</a></li>
<li class="show">Duncan, G.E., Leipzig, J.N., Mailman, R.B., and Lieberman, J.A. (1998). Differential effects of clozapine and haloperidol on ketamine-induced brain metabolic activation. Brain research 812, 65-75. <a href="https://doi.org/10.1016/S0006-8993(98)00926-3">https://doi.org/10.1016/S0006-8993(98)00926-3 </a></li>
<li class="show">El-Sisi, S., El-Nabarawy, S., Radwan, O., Abdel-Razek, A. (2015). Comparative Study of Some Natural and Artificial Food Coloring Agents on Hyperactivity, Learning and Memory Performance in Weanling Rats. In International Journal of Sciences: Basic and Applied Research (IJSBAR) (North America).</li>
<li class="show">Goldstein, J. (1999). Quetiapine fumarate (Seroquel): a new atypical antipsychotic. Drugs of today (Barcelona, Spain: 1998) 35, 193-210. <a href="https://doi.org/10.1358/dot.1999.35.3.533849">https://doi.org/10.1358/dot.1999.35.3.533849</a></li>
<li class="show">Hamon, M., and Blier, P. (2013). Monoamine neurocircuitry in depression and strategies for new treatments. Progress in Neuro-Psychopharmacology and Biological Psychiatry 45, 54-63. <a href="https://doi.org/10.1016/j.pnpbp.2013.04.009">https://doi.org/10.1016/j.pnpbp.2013.04.009 </a></li>
<li class="show">Hardwick, J.M., and Soane, L. (2013). Multiple functions of BCL-2 family proteins. Cold Spring Harbor perspectives in biology 5, a008722. <a href="https://doi.org/10.1101/cshperspect.a008722">https://doi.org/10.1101/cshperspect.a008722</a></li>
<li class="show">Heinrikson, R.L., and Meredith, S.C. (1984). Amino acid analysis by reverse-phase high-performance liquid chromatography: precolumn derivatization with phenylisothiocyanate. Analytical biochemistry 136, 65-74. <a href="https://doi.org/10.1016/0003-2697(84)90307-5">https://doi.org/10.1016/0003-2697(84)90307-5</a></li>
<li class="show">Kreuter, J. (2001). Nanoparticulate systems for brain delivery of drugs. Advanced drug delivery reviews 47, 65-81. <a href="https://doi.org/10.1016/S0169-409X(00)00122-8">https://doi.org/10.1016/S0169-409X(00)00122-8</a></li>
<li class="show">Krystal, J.H., Karper, L.P., Seibyl, J.P., Freeman, G.K., Delaney, R., Bremner, J.D., Heninger, G.R., Bowers, M.B., and Charney, D.S. (1994). Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans: psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Archives of general psychiatry 51, 199-214. <a href="https://doi.org/10.1001/archpsyc.1994.03950030035004">https://doi.org/10.1001/archpsyc.1994.03950030035004</a></li>
<li class="show">Levey, A.S., Coresh, J., Greene, T., Marsh, J., Stevens, L.A., Kusek, J.W., and Van Lente, F. (2007). Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clinical chemistry 53, 766-772. <a href="https://doi.org/10.1373/clinchem.2006.077180">https://doi.org/10.1373/clinchem.2006.077180</a></li>
<li class="show">Lodge, D.J., and Grace, A.A. (2011). Developmental pathology, dopamine, stress and schizophrenia. International Journal of Developmental Neuroscience 29, 207-213. <a href="https://doi.org/10.1016/j.ijdevneu.2010.08.002">https://doi.org/10.1016/j.ijdevneu.2010.08.002</a></li>
<li class="show">Maeshima, H., Ohnuma, T., Sakai, Y., Shibata, N., Baba, H., Ihara, H., Higashi, M., Ohkubo, T., Nozawa, E., and Abe, S. (2007). Increased plasma glutamate by antipsychotic medication and its relationship to glutaminase 1 and 2 genotypes in schizophrenia—Juntendo University Schizophrenia Projects (JUSP). Progress in Neuro-Psychopharmacology and Biological Psychiatry 31, 1410-1418. <a href="https://doi.org/10.1016/j.pnpbp.2007.06.009">https://doi.org/10.1016/j.pnpbp.2007.06.009</a></li>
<li class="show">Malhotra, A.K., Pinals, D.A., Adler, C.M., Elman, I., Clifton, A., Pickar, D., and Breier, A. (1997). Ketamine-induced exacerbation of psychotic symptoms and cognitive impairment in neuroleptic-free schizophrenics. Neuropsychopharmacology 17, 141-150. <a href="https://doi.org/10.1016/S0893-133X(97)00036-5">https://doi.org/10.1016/S0893-133X(97)00036-5</a></li>
<li class="show">Malhotra, A.K., Pinals, D.A., Weingartner, H., Sirocco, K., Missar, C.D., Pickar, D., and Breier, A. (1996). NMDA receptor function and human cognition: the effects of ketamine in healthy volunteers. Neuropsychopharmacology 14, 301-307. <a href="https://doi.org/10.1016/0893-133X(95)00137-3">https://doi.org/10.1016/0893-133X(95)00137-3</a></li>
<li class="show">McLamb, R.L., Williams, L.R., Nanry, K.P., Wilson, W.A., and Tilson, H.A. (1990). MK-801 impedes the acquisition of a spatial memory task in rats. Pharmacology Biochemistry and Behavior 37, 41-45. <a href="https://doi.org/10.1016/0091-3057(90)90038-J">https://doi.org/10.1016/0091-3057(90)90038-J</a></li>
<li class="show">Mehnert, W., and Mäder, K. (2001). Solid lipid nanoparticles: production, characterization and applications. Advanced drug delivery reviews 47, 165-196. <a href="https://doi.org/10.1016/S0169-409X(01)00105-3">https://doi.org/10.1016/S0169-409X(01)00105-3</a></li>
<li class="show">Meyer, J.M., and Koro, C.E. (2004). The effects of antipsychotic therapy on serum lipids: a comprehensive review. Schizophrenia research 70, 1-17. <a href="https://doi.org/10.1016/j.schres.2004.01.014">https://doi.org/10.1016/j.schres.2004.01.014</a></li>
<li class="show">MuÈller, R.H., MaÈder, K., and Gohla, S. (2000). Solid lipid nanoparticles (SLN) for controlled drug delivery–a review of the state of the art. European journal of pharmaceutics and biopharmaceutics 50, 161-177. <a href="https://doi.org/10.1016/S0939-6411(00)00087-4">https://doi.org/10.1016/S0939-6411(00)00087-4</a></li>
<li class="show">Narala, A., and Veerabrahma, K. (2013). Preparation, characterization and evaluation of quetiapine fumarate solid lipid nanoparticles to improve the oral bioavailability. Journal of pharmaceutics 2013. <a href="https://doi.org/10.1155/2013/265741">https://doi.org/10.1155/2013/265741</a></li>
<li class="show">Olesen, J., Gustavsson, A., Svensson, M., Wittchen, H.U., and Jönsson, B. (2012). The economic cost of brain disorders in Europe. European journal of neurology 19, 155-162. <a href="https://doi.org/10.1111/j.1468-1331.2011.03590.x">https://doi.org/10.1111/j.1468-1331.2011.03590.x</a></li>
<li class="show">Pagel, P., Blome, J., and Wolf, H.U. (2000). High-performance liquid chromatographic separation and measurement of various biogenic compounds possibly involved in the pathomechanism of Parkinson's disease. Journal of Chromatography B: Biomedical Sciences and Applications 746, 297-304. <a href="https://doi.org/10.1016/S0378-4347(00)00348-0">https://doi.org/10.1016/S0378-4347(00)00348-0</a></li>
<li class="show">Panel, N.N.C.E.P.E. (2001). Third report of the MCEP. Evaluation and treatment of high blood cholesterol in adults (Bethesda National Heart, lung and blood institute.).</li>
<li class="show">Parvanthi, M., Prathyusha, A., Kiran, R., and Reddy, J.R. (2014). Preparation and evaluation of quetiapine fumarate microemulsions: A novel delivery system. Asian J Pharm Clin Res 7, 208-213.</li>
<li class="show">Pickard, B.S. (2015). Schizophrenia biomarkers: translating the descriptive into the diagnostic. Journal of Psychopharmacology 29, 138-143. <a href="https://doi.org/10.1177/0269881114566631">https://doi.org/10.1177/0269881114566631</a></li>
<li class="show">Rathi, M.G., S; Seth, AK and Sachinkumar, PC (2013). Development and characterization of quetiapine looded chitosan nanoparticle. Pharma Science Monitor 4, 150-169.</li>
<li class="show">Redrobe, J.P., Elster, L., Frederiksen, K., Bundgaard, C., de Jong, I.E., Smith, G.P., Bruun, A.T., Larsen, P.H., and Didriksen, M. (2012). Negative modulation of GABAA α5 receptors by RO4938581 attenuates discrete sub-chronic and early postnatal phencyclidine (PCP)-induced cognitive deficits in rats. Psychopharmacology 221, 451-468. <a href="https://doi.org/10.1007/s00213-011-2593-9">https://doi.org/10.1007/s00213-011-2593-9</a></li>
<li class="show">Riedel, M., Müller, N., Strassnig, M., Spellmann, I., Severus, E., and Möller, H.-J. (2007). Quetiapine in the treatment of schizophrenia and related disorders. Neuropsychiatric disease and treatment 3, 219. <a href="https://doi.org/10.2147/nedt.2007.3.2.219">https://doi.org/10.2147/nedt.2007.3.2.219 </a></li>
<li class="show">Schumann, G., Canalias, F., Joergensen Poul, J., Kang, D., Lessinger, J.-M., Klauke, R., and on behalf of the Committee on Reference Systems for, E. (2010). IFCC reference procedures for measurement of the catalytic concentrations of enzymes: corrigendum, notes and useful advice. In Clinical Chemistry and Laboratory Medicine, pp. 615.<a href=" https://doi.org/10.1515/CCLM.2010.137"> https://doi.org/10.1515/CCLM.2010.137</a></li>
<li class="show">Sweetman, S. (2007). Martindle, the complete Drug reference, 35 edn (London: Pharmaceutical Press).</li>
<li class="show">Tietz, N. (1994). Fundaments of Clinical Chemistry, 2 edn.</li>
<li class="show">Tietz, N. (1995). Clinical guide to laboratory tests, 3 edn (AACC).</li>
<li class="show">Tietz, N. (2005). The text book of clinical chemistry and molecular diagnosis (4th edn) Burtis.</li>
<li class="show">Ashwood and Bruns (Eds) Elsevier Saunders 2290. Tsai, G., and Coyle, J.T. (2002). Glutamatergic mechanisms in schizophrenia. Annual review of pharmacology and toxicology 42, 165-179. <a href="https://doi.org/10.1146/annurev.pharmtox.42.082701.160735 ">https://doi.org/10.1146/annurev.pharmtox.42.082701.160735 </a></li>
<li class="show">Van den Buuse, M., and de Jong, W. (1989). Differential effects of dopaminergic drugs on open-field behavior of spontaneously hypertensive rats and normotensive Wistar-Kyoto rats. Journal of Pharmacology and Experimental Therapeutics 248, 1189-1196.</li>
<li class="show">Wang, Y.-C., Ho, U.-C., Ko, M.-C., Liao, C.-C., and Lee, L.-J. (2012). Differential neuronal changes in medial prefrontal cortex, basolateral amygdala and nucleus accumbens after postweaning social isolation. Brain Structure and Function 217, 337-351. <a href="https://doi.org/10.1007/s00429-011-0355-4">https://doi.org/10.1007/s00429-011-0355-4</a></li>
<li class="show">Yang, X.-C., and Reis, D.J. (1999). Agmatine selectively blocks then-methyl-d-aspartate subclass of glutamate receptor channels in rat hippocampal neurons. Journal of Pharmacology and Experimental Therapeutics 288, 544-549.</li>
</ol>
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.