Psychosocial adjustment to cancer and its associated factors in patients undergoing chemotherapy: A cross-sectional study
DOI:
https://doi.org/10.15419/bmrat.v4i12.392Keywords:
Adjustment, Cancer, Chemotherapy, medicineAbstract
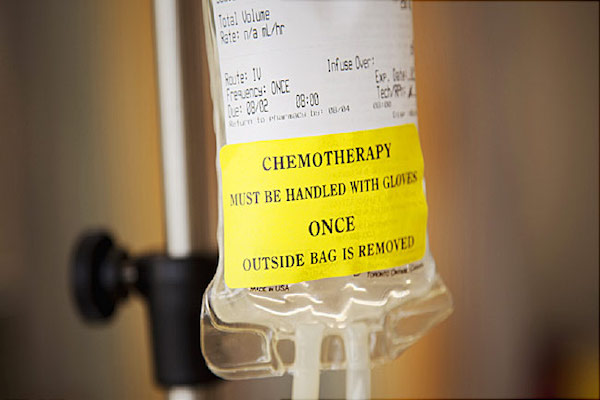
Background: Adjustment to cancer refers to functions adopted by an individual for sustaining health and well-being, and leads to a better life and improved quality of life. Failure to adjust causes anxiety, depression, distress, and behavioral problems. The aim of study was to assess psychosocial adjustment to cancer and its associated factors in patients undergoing chemotherapy.
Methods: This cross-sectional study recruited 260 cancer patients undergoing chemotherapy at a hospital center in Kashan, Iran in 2016. Data collection tools included demographic details, Psychological Adjustment to Illness Scale (PAIS), and adherence to religious beliefs (Temple). Samples were selected by convenience sampling method. Data were analyzed in SPSS-16 software using descriptive statistics, Chi-square test, and Pearson’s correlation coefficient.
Results: The mean age of participants was 54.76±13.82 years, duration with cancer was 10.11±18.89 months, duration of treatment with chemotherapy was 4.8±6.2 months, and the mean score adjustment was 50.1±17.18. Adjustment was found to be significantly related to education, marital status, financial status, employment, and adherence to religious beliefs, but not to age, duration with cancer, duration of chemotherapy, or place of residence. Patients with no metastasis were better adjusted compared to other groups, with a significant difference from the other groups.
Conclusion: More than half of patients had moderate to high levels of adjustment. Patients with poor education, self-employment, no family support, low adherence to religious beliefs, and with metastasis displayed poorer adjustment levels; all of these negatively affected their adjustment to cancer. Thus, patients undergoing chemotherapy need greater family, social, and economic support for adjustment.
References
<li>Akbari, M. (2013). Effectiveness of Mindfulness Training in Decreasing the Perceived Stress among the Patients Suffering from Breast Cancer. Journal of Thought & Behavior in Clinical Psychology., 7(27), 7–16.</li>
<li>Momeni, T., Musarezaie, A., Karimian, J., Ebrahimi, A., . . .. (2012). The relationship between spiritual well-being and depression in Iranian breast cancer patients. Health Information Management, (0): 524.</li>
<li>Rajabpour, H., & Tavakolizadeh, J. (2012). The relationship between emotional intelligence and adjusment in cancer patients in Mashhad. The Horizon of Medical Sciences., 18(1), 17–25.</li>
<li>Zemestani, M., Hasannejad, L., & Nejadian, A. (2013). Comparison of quality of life, sleep quality and social adjustment of cancerous patients with intact individual in Ahvaz city. Majallah-i Pizishki-i Urumiyyah, 24(7), 471–482.</li>
<li>Sadjadian, A., Haghghat, S., Montazeri, A., Kazemnedjad, A., & Alavinili, A. (2011). Post diagnosis coping strategies patients with breast cancer. Iranian Journal of Breast Disease., 4(3), 52–58.</li>
<li>Ahangar, R., Parvan, K., Hosseini, F. A., Abdollahzadeh, F., Seyedrasooli, E., & Ghojazadeh, M. (2013). Stressors and coping methods of patients on hemodialysis in Tabriz Imam Reza teaching hospital in 2009. Razi Journal of Medical Sciences., 20(111), 1–11.</li>
<li>Samadzade, N., Poursharifi, H., and Babapour, J. (2015). The effectiveness of cognitive-behavioral therapy on the psycho-social adjustment to illness and symptoms of depression in individuals with type ii diabetes. Quarterly Clinical Psychology Studies 5, 77 -96.</li>
<li>Markani, A. K., Fard, M. K., Yaghmaei, F., Abbasi, M., & Didarloo, A. (2016). Spirituality as Experienced by Iranian Muslim Oncology Nurses; A qualitative study. History of Medicine Journal (Quarterly), 6(21), 185–209.</li>
<li>Trevino, K. M., Balboni, M., Zollfrank, A., Balboni, T., & Prigerson, H. G. (2014). Negative religious coping as a correlate of suicidal ideation in patients with advanced cancer. Psycho-Oncology, 23(8), 936–945. <a href="https://doi.org/10.1002/pon.3505">https://doi.org/10.1002/pon.3505</a></li>
<li>D’Souza, C.A., Antony, S., Thomas, B., and Murthy, S.G. (2016). Coping strategies used by cancer patients to deal with physical and psychological problems of chemotherapy. International Journal of Innovative Research and Development 5, 36-41.</li>
<li>Drageset, S., Lindstrøm, T. C., & Underlid, K. (2016). “I just have to move on”: Women’s coping experiences and reflections following their first year after primary breast cancer surgery. European Journal of Oncology Nursing, 21, 205–211. <a href="https://doi.org/10.1016/j.ejon.2015.10.005">https://doi.org/10.1016/j.ejon.2015.10.005</a></li>
<li>Shapiro, J. P., McCue, K., Heyman, E. N., Dey, T., & Haller, H. S. (2010). A naturalistic evaluation of psychosocial interventions for cancer patients in a community setting. Journal of Psychosocial Oncology, 28(1), 23–42. <a href="https://doi.org/10.1080/07347330903438891">https://doi.org/10.1080/07347330903438891</a></li>
<li>Gonzalez, P., Nuñez, A., Wang-Letzkus, M., Lim, J.-W., Flores, K. F., & Nápoles, A. M. (2016). Coping with breast cancer: Reflections from Chinese American, Korean American, and Mexican American women. Health Psychology, 35(1), 19–28. <a href="https://doi.org/10.1037/hea0000263">https://doi.org/10.1037/hea0000263</a></li>
<li>Gonzales, F. A., Hurtado‐de‐Mendoza, A., Santoyo‐Olsson, J., & Nápoles, A. M. (2015). Do coping strategies mediate the effects of emotional support on emotional well‐being among Spanish‐speaking Latina breast cancer survivors? Psycho-Oncology.</li>
<li>Hund, B., Reuter, K., Härter, M., Brähler, E., Faller, H., Keller, M., . . . Mehnert, A. (2016). stressors, symptom profile, and predictors of adjustment disorder in cancer patients. results from an epidemiological study with the composite international diagnostic interview, adaptation for oncology (cidi‐o). Depression and Anxiety, 33(2), 153–161. <a href="https://doi.org/10.1002/da.22441">https://doi.org/10.1002/da.22441</a></li>
<li>Brunault, P., Champagne, A. L., Huguet, G., Suzanne, I., Senon, J. L., Body, G., . . .. (2015). Major depressive disorder, personality disorders, and coping strategies are independent risk factors for lower quality of life in non‐metastatic breast cancer patients. Psycho-Oncology.</li>
<li>Mehri Nejad, S.A., Ramezan Saatchi, L., and Paydar, S. (2017). Death Anxiety and Its Relationship with Social Support and Adherence to Religion in the Elderly. Iranian Journal of Ageing 11, 494-503.</li>
<li>Koenig, H. G. (2007). Spirituality and depression: A look at the evidence. Southern Medical Journal, 100(7), 737–740. https://doi.org/10.1097/SMJ.0b013e318073c68c</li>
<li>Jim, H. S., Pustejovsky, J. E., Park, C. L., Danhauer, S. C., Sherman, A. C., Fitchett, G., . . . Salsman, J. M. (2015). Religion, spirituality, and physical health in cancer patients: A meta‐analysis. Cancer, 121(21), 3760–3768. <a href="https://doi.org/10.1002/cncr.29353">https://doi.org/10.1002/cncr.29353</a></li>
<li>Weaver, A. J., & Flannelly, K. J. (2004). The role of religion/spirituality for cancer patients and their caregivers. Southern Medical Journal, 97(12), 1210–1214. <a href="https://doi.org/10.1097/01.SMJ.0000146492.27650.1C">https://doi.org/10.1097/01.SMJ.0000146492.27650.1C</a></li>
<li>Ahmadi, F., & Ahmadi, N. (2015). Nature as the most important coping strategy among cancer patients: A Swedish survey. Journal of Religion and Health, 54(4), 1177–1190. <a href="https://doi.org/10.1007/s10943-013-9810-2">https://doi.org/10.1007/s10943-013-9810-2</a></li>
<li>Vellone, E., Rega, M. L., Galletti, C., & Cohen, M. Z. (2006). Hope and related variables in Italian cancer patients. Cancer Nursing, 29(5), 356–366. <a href="https://doi.org/10.1097/00002820-200609000-00002">https://doi.org/10.1097/00002820-200609000-00002</a></li>
<li>Paiva, C. E., Paiva, B. S. R., de Castro, R. A., de Pádua Souza, C., de Paiva Maia, Y. C., Ayres, J. A., . . .. (2013). A pilot study addressing the impact of religious practice on quality of life of breast cancer patients during chemotherapy. Journal of Religion and Health, 52(1), 184–193. <a href="https://doi.org/10.1007/s10943-011-9468-6">https://doi.org/10.1007/s10943-011-9468-6</a></li>
<li>Assimakopoulos, K., Karaivazoglou, K., Ifanti, A. A., Gerolymos, M. K., Kalofonos, H. P., & Iconomou, G. (2009). Religiosity and its relation to quality of life in Christian Orthodox cancer patients undergoing chemotherapy. Psycho-Oncology, 18(3), 284–289. <a href="https://doi.org/10.1002/pon.1402">https://doi.org/10.1002/pon.1402</a></li>
<li>Taghavi, M., Kalafi, E., Talei, A., Dehbozorgi, G., & Taghavi, S. M. A. (2011). Investigating the Relation of Depression and Religious Coping and Social Support in Women with Breast Cancer. Majallah-i Danishkadah Pizishki-i Isfahan, 28(115).</li>
<li>Feghhi, H., Saadatjoo, A., & Dastjerdi, R. (2014). Psychosocial adaptation in patients with type 2 diabetes referring to Diabetes Research Center of Birjand in 2013. Modern Care Journal., 10(4), 249–256.</li>
<li>Jafari, E., Hajloo, N., & Mohammadzadeh, A. (2015). The Relationship between the Practice of Religious Beliefs, Spiritual Well Being, General Health and Coping Styles in Soldiers. Journal of Military Medicine., 16(4), 191–196.</li>
<li>Dempster, M., McCarthy, T., & Davies, M. (2011). Psychological adjustment to Type 2 diabetes and relationship quality. Diabetic Medicine, 28(4), 487–492. <a href="https://doi.org/10.1111/j.1464-5491.2010.03214.x">https://doi.org/10.1111/j.1464-5491.2010.03214.x</a></li>
<li>Grinstein, G., Muzumdar, R., Aponte, L., Vuguin, P., Saenger, P., & DiMartino-Nardi, J. (2003). Presentation and 5-year follow-up of type 2 diabetes mellitus in African-American and Caribbean-Hispanic adolescents. Hormone Research in Paediatrics, 60(3), 121–126. <a href="https://doi.org/10.1159/000072523">https://doi.org/10.1159/000072523</a></li>
<li>Kalilzade, H., Nanbakhsh, J., & Yaghobi, M. (2006). Check the compatibility of heart failure patients with complications of the disease in the Training Center - Taleghani Hospital in Urmia. Journal of Nursing and Midwifery Urmia University of Medical Sciences., 4(4), 154–160.</li>
<li>Tol, A., Majlessi, F., Rahimi, F.A., Shojaeezadeh, D., and Mohebbi, B. (2012). Factors associated with supportive and coping obstacles of adjustment with type II diabetes. Health System Research 8, 1088-1097.</li>
<li>Siston, A. K., List, M. A., Daugherty, C. K., Banik, D. M., Menke, C., Cornetta, K., & Larson, R. A., & the Siston a. (2001). Psychosocial adjustment of patients and caregivers prior to allogeneic bone marrow transplantation. Bone Marrow Transplantation, 27(11), 1181–1188. <a href="https://doi.org/10.1038/sj.bmt.1703059">https://doi.org/10.1038/sj.bmt.1703059</a></li>
<li>De-Nour, A. K. (1982). Psychological adjustment to illness scale (PAIS): A study of chronic hemodialysis patients. Journal of Psychosomatic Research, 26(1), 11–22. <a href="https://doi.org/10.1016/0022-3999(82)90058-7">https://doi.org/10.1016/0022-3999(82)90058-7</a></li>
<li>Sodagar, S., Ahadi, H., Jomehri, F., Rahgozar, M., & Jahani, M. (2013). Quality of Life and Physical well-being after bone marrow transplantation in patients with acute leukaemia. [J Kermanshah Univ Med Sci]. Majallah-i Danishgah-i Ulum-i Pizishki-i Kirmanshah, 16(8), 610–616.</li>
<li>Elahi, N., Kaardani, M., Alhani, F., & Tali, S. (2015). Transplantation living with mastectomy: Explaining the experiences adaptation with mastectomy of young women undergoing chemotherapy. Journal of Urmia Nursing And Midwifery Faculty., 12(10), 908–918.</li>
<li>Vallurupalli, M. M., Lauderdale, M. K., Balboni, M. J., Phelps, A. C., Block, S. D., Ng, A. K., . . . Balboni, T. A. (2012). The role of spirituality and religious coping in the quality of life of patients with advanced cancer receiving palliative radiation therapy. The Journal of Supportive Oncology, 10(2), 81–87. <a href="https://doi.org/10.1016/j.suponc.2011.09.003">https://doi.org/10.1016/j.suponc.2011.09.003</a></li>
<li>Rezaei, M., Seyedfatemi, N., and Hosseini, F. (2008). Spiritual Well-being in Cancer Patients who Undergo Chemotherapy. Hayat 14, 104-104.</li>
<li>Zamanzadeh, V., Rassouli, M., Abbaszadeh, A., Nikanfar, A.-R., Alavi-Majd, H., Mirza-Ahmadi, F., . . .. (2014). Spirituality in cancer care: A qualitative study. Journal of Qualitative Research in Health Sciences., 2(4), 366–378.</li>
<li>Jani, S., & Molaee, M. (2014). JANGI GS, Pouresmali A. Effectiveness of Cognitive Therapy Based on Religious Believes on Death Anxiety. Social Adjustment and Subjective Well-being in the Cancer Patients.</li>
</ol>
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
