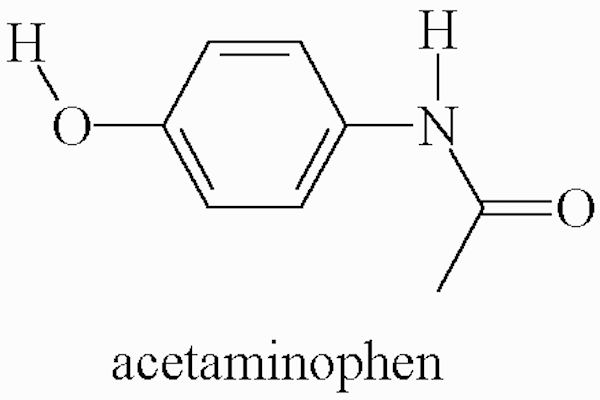
Closure of patent ductus arteriosus with oral acetaminophen in preterm neonates: A randomized trial
DOI:
https://doi.org/10.15419/bmrat.v5i02.418Keywords:
Acetaminophen (Paracetamol), Neonates, Patent Ductus ArteriosusAbstract
Introduction: Patent ductus arteriosus (PDA) is one of the most common cardiac problems in preterm neonates which could lead to morbidities, such as chronic lung disease, intraventricular hemorrhage and retinopathy. The aim of this study was to evaluate the effect of oral acetaminophen on closure of PDA in preterm neonates.
Methods: Sixty-nine neonates with significant PDA (confirmed through echocardiography) were recruited in this study. Ibuprofen and indomethacin were contraindicated in these neonates These newborns were randomly divided into two groups of cases (n=36) and controls (n=33). The case group was treated with oral acetaminophen at a dose of 15 mg/kg/dose every 6 hours for 72 hours. The control group did not receive any intervention. After 72 hours, both groups were re-evaluated by echocardiography. In case of failed closure of PDA, the second course of treatment would be administration of acetaminophen. The main outcome of this study was to evaluate the rate of closure of PDA and the side effects of the acetaminophen.
Results: The overall rate of PDA closure in the acetaminophen-receiving group was 94.4%; the ductus arteriosus was closed in 75% of patients with the first course of treatment. Moreover, 19.4% of patients did not respond to the first course of the treatment but their ductus arteriosus was closed with the second course of acetaminophen treatment. Of the patients, 5.6% did not respond to both courses of acetaminophen treatments. For the control group, the closure rate of PDA was 15.1%.
Conclusion: The results of the study showed that oral acetaminophen is an effective alternative treatment for PDA in preterm neonates.
References
Anderson, B. J. (2008). Paracetamol (Acetaminophen): Mechanisms of action. Paediatric Anaesthesia, 18(10), 915–921. https://doi.org/10.1111/j.1460-9592.2008.02764.x PMID:18811827Bose, C. L., & Laughon, M. M. (2007). Patent ductus arteriosus: Lack of evidence for common treatments. Archives of Disease in Childhood. Fetal and Neonatal Edition, 92(6), F498–F502. https://doi.org/10.1136/adc.2005.092734 PMID:17951552
Clyman RI, Couto J, Murphy GM. Patent ductus arteriosus: are current neonatal treatment options better or worse than no treatment at all? Seminars in perinatology, 2012. Elsevier, 123-9. https://doi.org/10.1053/j.semperi.2011.09.022
Dang, D., Wang, D., Zhang, C., Zhou, W., Zhou, Q., & Wu, H. (2013). Comparison of oral paracetamol versus ibuprofen in premature infants with patent ductus arteriosus: A randomized controlled trial. PLoS One, 8(11), e77888. https://doi.org/10.1371/journal.pone.0077888 PMID:24223740
DeMauro, S. B., & Wright, C. J. (2014). Acetaminophen: A possible alternative to ibuprofen in patent ductus arteriosus closure. The Journal of Pediatrics, 165(1), 209–210. https://doi.org/10.1016/j.jpeds.2014.04.025 PMID:24973162
Dollberg, S., Lusky, A., & Reichman, B. (2005). Patent ductus arteriosus, indomethacin and necrotizing enterocolitis in very low birth weight infants: A population-based study. Journal of Pediatric Gastroenterology and Nutrition, 40(2), 184–188. https://doi.org/10.1097/00005176-200502000-00019 PMID:15699694
George, I., Mekahli, D., Rayyan, M., Levtchenko, E., & Allegaert, K. (2011). Postnatal trends in creatinemia and its covariates in extremely low birth weight (ELBW) neonates. Pediatric Nephrology (Berlin, Germany), 26(10), 1843–1849. https://doi.org/10.1007/s00467-011-1883-0 PMID:21499946
Gournay, V. (2011). The ductus arteriosus: Physiology, regulation, and functional and congenital anomalies. Archives of Cardiovascular Diseases, 104(11), 578–585. https://doi.org/10.1016/j.acvd.2010.06.006 PMID:22117910
Grèen, K., Drvota, V., & Vesterqvist, O. (1989). Pronounced reduction of in vivo prostacyclin synthesis in humans by acetaminophen (paracetamol). Prostaglandins, 37(3), 311–315. https://doi.org/10.1016/0090-6980(89)90001-4 PMID:2664901
Hammerman, C., Bin-Nun, A., Markovitch, E., Schimmel, M. S., Kaplan, M., & Fink, D. (2011). Ductal closure with paracetamol: A surprising new approach to patent ductus arteriosus treatment. Pediatrics, 128(6), e1618–e1621. https://doi.org/10.1542/peds.2011-0359 PMID:22065264
Jones L, Craven P, Attia J, et al (2010). Network meta-analysis of indomethacin versus ibuprofen versus placebo for PDA in preterm infants. Archives of Disease in Childhood-Fetal and Neonatal Edition, fetalneonatal168682.
Koch, J., Hensley, G., Roy, L., Brown, S., Ramaciotti, C., & Rosenfeld, C. R. (2006). Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or less. Pediatrics, 117(4), 1113–1121. https://doi.org/10.1542/peds.2005-1528 PMID:16585305
Le, J., Gales, M. A., & Gales, B. J. (2015). Acetaminophen for patent ductus arteriosus. The Annals of Pharmacotherapy, 49(2), 241–246. https://doi.org/10.1177/1060028014557564 PMID:25352038
Lucas, R., Warner, T. D., Vojnovic, I., & Mitchell, J. A. (2005). Cellular mechanisms of acetaminophen: Role of cyclo-oxygenase. The FASEB Journal, 19(6), 635–637. https://doi.org/10.1096/fj.04-2437fje PMID:15705740
Nadir, E., Kassem, E., Foldi, S., Hochberg, A., & Feldman, M. (2014). Paracetamol treatment of patent ductus arteriosus in preterm infants. Journal of Perinatology, 34(10), 748–749. https://doi.org/10.1038/jp.2014.96 PMID:24854626
Oncel, M. Y., Yurttutan, S., Degirmencioglu, H., Uras, N., Altug, N., Erdeve, O., & Dilmen, U. (2013). Intravenous paracetamol treatment in the management of patent ductus arteriosus in extremely low birth weight infants. Neonatology, 103(3), 166–169. https://doi.org/10.1159/000345337 PMID:23258386
Oncel MY, Yurttutan S, Erdeve O, et al (2014). Oral paracetamol versus oral ibuprofen in the management of patent ductus arteriosus in preterm infants: a randomized controlled trial. The Journal of pediatrics, 164, 510-4. e1. https://doi.org/10.1016/j.jpeds.2013.11.008
Sancak, S., Gokmen Yildirim, T., Topcuoglu, S., Yavuz, T., Karatekin, G., & Ovali, F. (2016). Oral versus intravenous paracetamol: Which is better in closure of patent ductus arteriosus in very low birth weight infants? The Journal of Maternal-Fetal & Neonatal Medicine, 29(1), 135–139. https://doi.org/10.3109/14767058.2014.989829 PMID:25471090
Sinha, R., Negi, V., & Dalal, S. S. (2013). An interesting observation of PDA closure with oral paracetamol in preterm neonates. Journal of Clinical Neonatology, 2(1), 30–32. https://doi.org/10.4103/2249-4847.109245 PMID:24027742
Soligard, H. T., Nilsen, O. G., & Bratlid, D. (2010). Displacement of bilirubin from albumin by ibuprofen in vitro. Pediatric Research, 67(6), 614–618. https://doi.org/10.1203/PDR.0b013e3181da7578 PMID:20216106
Sutherland, M. R., Yoder, B. A., McCurnin, D., Seidner, S., Gubhaju, L., Clyman, R. I., & Black, M. J. (2012). Effects of ibuprofen treatment on the developing preterm baboon kidney. American Journal of Physiology. Renal Physiology, 302(10), F1286–F1292. https://doi.org/10.1152/ajprenal.00216.2011 PMID:22357916
Tekgündüz, K. Ş., Ceviz, N., Caner, İ., Olgun, H., Demirelli, Y., Yolcu, C., . . . Kara, M. (2015). Intravenous paracetamol with a lower dose is also effective for the treatment of patent ductus arteriosus in pre-term infants. Cardiology in the Young, 25(6), 1060–1064. https://doi.org/10.1017/S1047951114001577 PMID:25160728
Vieux R, Fresson J, Guillemin F, et al (2010). Perinatal drug exposure and renal function in very preterm infants. Archives of Disease in Childhood-Fetal and Neonatal Edition, fetalneonatal197699.
Yurttutan, S., Oncel, M. Y., Arayicı, S., Uras, N., Altug, N., Erdeve, O., & Dilmen, U. (2013). A different first-choice drug in the medical management of patent ductus arteriosus: Oral paracetamol. The Journal of Maternal-Fetal & Neonatal Medicine, 26(8), 825–827. https://doi.org/10.3109/14767058.2012.755162 PMID:23205872
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
