Elevated levels of circulating soluble ST2 at discharge predict late adverse ventricular remodeling in patients with ST-segment elevation myocardial infarction
DOI:
https://doi.org/10.15419/bmrat.v5i12.505Keywords:
Cardiac remodeling, Percutaneous coronary intervention, Prediction, Soluble ST2, ST-segment elevation myocardial infarctionAbstract
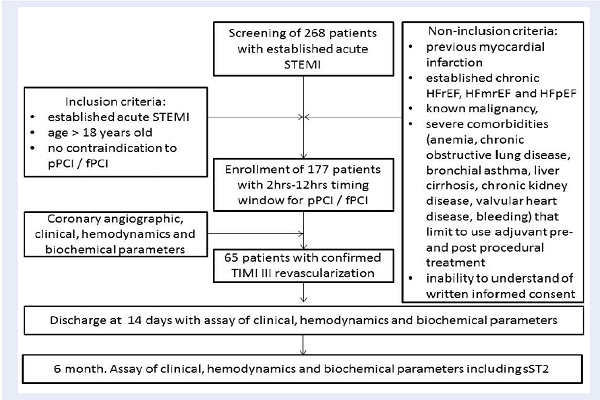
Introduction: The aim of this study was to investigate whether the circulating level of sST2 would predict adverse LV remodeling in STEMI patients with TIMI III flow through the myocardial infarctrelated coronary artery six months after intervention.
Methods: The study retrospectively included 65 patients with STEMI and TIMI-III flow after primary or facilitated percutaneous coronary intervention (PCI). These patients were admitted to the intensive care unit of L.T. Malaya Therapy National Institute between August 2016 and July 2018. Primary PCI with bare-metal stent implantation was performed in 33 patients, and 32 patients were previously treated with primary thrombolysis followed by PCI within 12 hours after initial STEMI confirmation. Angiographic, clinical, and biochemical parameters were evaluated. B-mode, Tissue Doppler, Strain Echocardiography, and blood sampling for biomarker assays were performed at admission, at discharge from the hospital, and at six months after STEMI.
Results: Late adverse LV remodeling is defined as an increase of LV end-diastolic volume (EDV) six months post STEMI (first cohort, n=29), while other patients (second cohort, n=36) did not demonstrate a decreasing trend of LV EDV, or they had never revealed any decrease of this parameter. There was a significant difference between the two cohorts in the serum level of sST2 at discharge, while the levels of natriuretic peptides, troponin I were similar (P=0.24). Indeed, the circulating level of sST2 in the first cohort was higher than that of the second cohort (59.72 ng/mL; 95% confidence interval [CI] = 36.99 ng/mL -139.53 ng/mL versus 44.75 ng/mL; 95%CI =28.25 ng/mL -77.32 ng/mL, P=0.039, respectively). ROC-analyses showed that the best balanced cut-off point for sST2 to predict adverse remodeling at 6 months post PCI was 35 ng/mL (AUC=0.672 95% C 0.523-0.799; P=0.0344 sensitivity = 46.7% and specificity = 85.7%).
Conclusions: We showed that the circulating level of sST2 measured at discharge in acute STEMI patients intervented by PCI could predict late adverse LV remodeling six months post PCI. These findings offer a new biomarker to stratify patients with successful coronary re-vascularization at risk of HF.
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
