Comparison of clinical outcome of frozen embryo transfer after embryo selection based on morphokinetic versus morphologic criteria for freezing
DOI:
https://doi.org/10.15419/bmrat.v5i12.510Keywords:
Embryo evaluation, Embryo selection, Morphologic, Morphokinetic, Time-lapseAbstract
Background: Results from the latest meta-analysis, in fresh cycles, showed that the application of time-lapse monitoring (TLM) together with an embryo-evaluating algorithm was associated with a significantly higher rate of ongoing pregnancy and a lower rate of early pregnancy loss. The aim of this study was to compare the clinical outcomes of frozen embryos classified according to morphokinetic versus morphologic criteria.
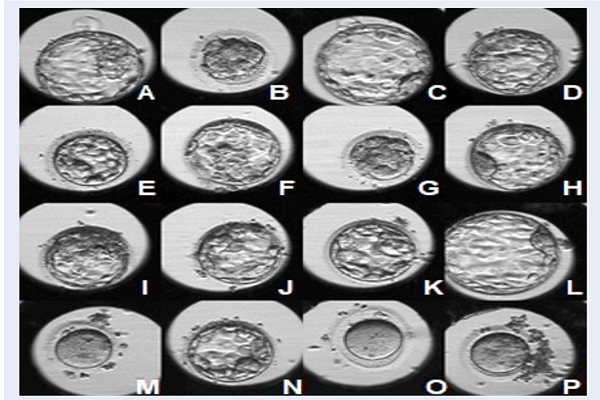
Methods: This was a retrospective cohort study, conducted at IVFAS, An Sinh Hospital, Vietnam, from July 2014 to July 2017. Patients undergoing in vitro fertilization (IVF) treatment with antagonist protocol and having freeze-only on day 5 were included. Exclusion criteria were patients (i) treated with in-vitro maturation, (ii) having obstructive azoospermia, or (iii) having uterine abnormalities. Embryos were cultured up to day 5 in TLM system (Primo Vision, Vitrolife, Sweden) or in benchtop (G185, K System, Denmark). The quality of frozen embryos was evaluated based on morphokinetic or morphologic criteria. In the subsequent cycle, endometrial preparation was done by using exogenous estradiol and progesterone. Embryos were thawed and up to 2 embryos were transferred to the uterus. The primary outcome was ongoing pregnancy. The rate of post-thaw survival, post-thawed good/moderate embryo, clinical pregnancy, implantation, miscarriage and ectopic pregnancy were used as secondary endpoints.
Results: A total of 276 patients were recruited, with 138 patients in the morphokinetic group and 138 patients in the morphologic group. Baseline characteristics were comparable between the two groups. There was no significant difference in ongoing pregnancy rate in morphokinetic versus morphologic group (57.2% vs. 60.1%, p=0.71). All secondary outcomes were comparable between the two groups.
Conclusion: In frozen day-5 embryo transfer, the clinical outcomes were similar when embryos were classified according to morphokinetic versus morphologic criteria for freezing. Using morphokinetic criteria to select embryos for freezing did not improve the ongoing pregnancy rate, as compared to morphologic criteria.
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
