The efficacy of adding vitamin B12 to pegylated interferon and ribavirin treatment in Hepatitis C virus patients regarding the host and viral prognostic factors
DOI:
https://doi.org/10.15419/bmrat.v6i2.524Keywords:
Hepatitis C virus, Pegylated Interferon, Ribavirin, Vitamin B12Abstract
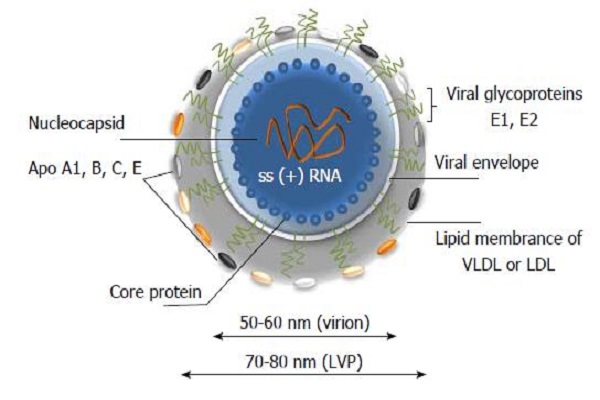
Introduction: Hepatitis C virus (HCV) infection affects almost 180 million people around the world. Even though the development of direct acting antivirals (DAAs) has significantly improved the treatment responses to HCV infection, treatment with pegylated interferon (PegIFN) in combination with ribavirin is considered the standard of care (SOC) for chronic HCV infection treatment in countries with limited medical resources. Considering the inhibitory effect of vitamin B12 on HCV replication, we have evaluated the effect of vitamin B12 supplementation along with SOC on treatment outcomes in patients with chronic HCV infection, who were antiviral treatment-naive.
Methods: In this regard, seventy-four HCV-infected patients, naïve to antiviral therapy, were randomly assigned to receive SOC or SOC in addition to vitamin B12 (SOC + B12). Viral response was evaluated at 4, 12, 24 and 48 weeks following the initiation of viral treatment and at 24 weeks after completing the treatment. Genotyping of the interleukin 28B (IL28B) polymorphisms was also performed. Demographic characteristics, clinical findings, fibroscan results and drug adverse effects were recorded.
Results: Our findings showed that rapid viral response was not significantly different between the two groups; however, the rates of complete early viral response (cEVR) (p=0.033), end-of-treatment viral response (ETVR) (p=0.001) and sustained virologic response (SVR) (p=0.0001) were significantly higher in SOC + B12 patients compared to SOC patients. Besides, in SOC + B12 patients, those with a higher baseline viral load and carriers of IL28B CC genotype showed significantly higher rate of SVR.
Conclusion: In conclusion, the addition of vitamin B12 significantly improved the rate of SVR in HCV-infected patients, who were naïve to antiviral therapy. As this treatment regimen is safe and inexpensive, it proposes an option for improving the effectiveness of the HCV treatment with SOC, particularly in resource-limited settings.
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
