Prevalence, treatment, and 1-year outcomes of heart failure with mid-range ejection fraction
DOI:
https://doi.org/10.15419/bmrat.v9i8.758Keywords:
Asian population, Clinical characteristics, GDMT, Heart failure, HFmrEF, outcomesAbstract
Background: The prevalence of patients with heart failure with mid-range ejection fraction (HFmrEF) remains unchanged regardless of healthcare strategies. HFmrEF has mixed characteristics of heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF). The treatment of HFmrEF was recommended to be similar to the treatment of HFpEF in the 2016 guidelines of the European Society of Cardiology (ESC) but was changed to those of HFrEF in the 2021 version. Objective: To describe the clinical characteristics of inpatients with HFmrEF with a focus on treatment practices.
Methods: A prospective study was conducted on patients diagnosed with HFmrEF who were admitted to the cardiology department of Nhan Dan Gia Dinh hospital from July 2019 to July 2020. Rehospitalization and mortality were followed up by telephone after 1 year.
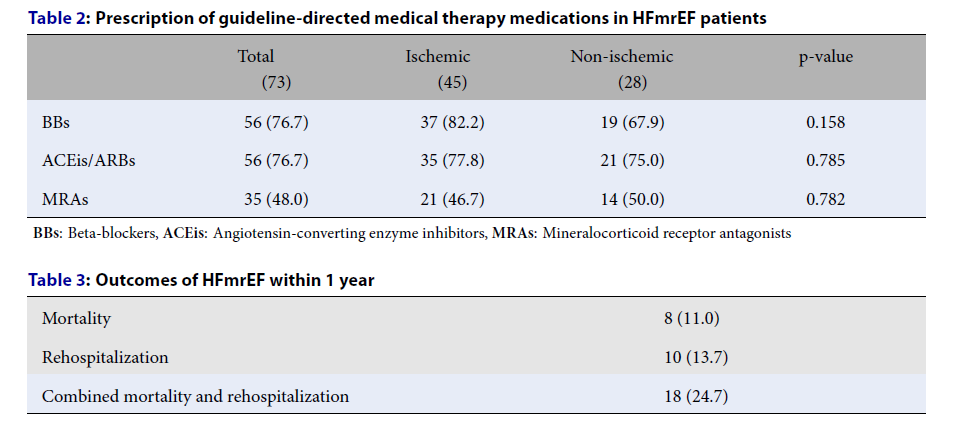
Results: Of a total of 529 heart failure cases admitted to the hospital during the study period, there were 73 patients (13.8%) with HFmrEF. The mean age was 68 years and males comprised 53%. The average hospitalization stay length was 6.7 days. The most common precipitating factors of heart failure were non-adherence (42.5%) and infection (39.7%) followed by hypertensive crisis (8.2%), anemia (6.8%), acute myocardial infarction (5.5%), arrhythmia (4.1%), and hyperthyroidism (2.7%). Ischemic heart disease was the leading cause (61.6%) of HFmrEF, followed by hypertension (12.3%). The rates of HFmrEF patients treated with beta-blockers, angiotensin-converting enzyme inhibitors, angiotensin II receptor antagonists, and aldosterone receptor antagonists were 76.1%, 76.71%, 37.73%, and 47.95%, respectively. There were no statistically significant differences in the guideline-directed medical therapy (GDMT) medications administered between HFmrEF due to ischemic and non-ischemic causes. After 1-year follow-up, the combined outcome of rehospitalization and mortality in HFmrEF was 24.7%.
Conclusion: The treatment of HFmrEF was similar to that of HFrEF between 2019 and 2020 at Nhan Dan Gia Dinh hospital and was in accordance with the 2021 ESC guidelines.
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.