Immunophenotypic Expression and its Association with Prognostic Factors, Clinical Stages, and Clinical Profiles in Newly Diagnosed Patients with Plasma Cell Myeloma: Insights from Two Tertiary Care Centers
DOI:
https://doi.org/10.15419/bmrat.v11i3.870Keywords:
Plasma cell myeloma, immunophenotypic, biochemical parameters, cytogenetic, molecular abnormalities, prognostic factors, clinical stagesAbstract
Objective: Plasma cell myeloma (PCM) is an incurable clonal neoplasm of plasma cells, which typically presents a poor prognosis. This study aimed to determine the clinical profile of newly diagnosed plasma cell myeloma cases in two tertiary care centers in Malaysia and evaluate the association of aberrant immunophenotypic expression with prognostic factors and clinical stages.
Methods: A four-year retrospective study of 78 newly diagnosed PCM cases was conducted at Hospital Kuala Lumpur (HKL) and Hospital Universiti Sains Malaysia (HUSM). The study retrieved data from medical records, including socio-demographic characteristics, hematological and biochemical parameters, cytogenetic and molecular abnormalities, immunophenotypic expression profile, and clinical stages of PCM cases. All data were statistically analyzed using SPSS 26.0.
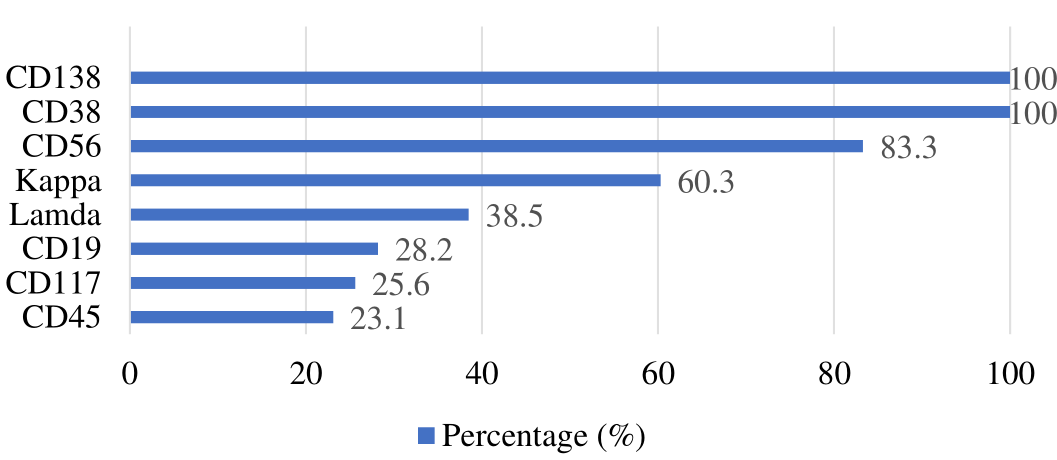
Results: The mean age of PCM patients was 60 years, with 73.1% of cases showing a normal white blood cell (WBC) count. A total of 65.4% and 24.4% of cases had anemia and mild to severe anemia, respectively. Cases were associated with thrombocytopenia (24.4%), normal platelet counts (75.6%), a bone marrow plasma cell percentage >10% (93.6%), and elevated erythrocyte sedimentation rate (ESR) (63.3%). Additionally, 66.7% of cases demonstrated hypoalbuminemia and elevated lactate dehydrogenase (LDH), calcium, and creatinine levels. All cases indicated hyperproteinemia (56.4%), hypoproteinemia (6.4%), normal serum total protein (37.2%), elevated serum paraprotein (69.2%), and blood beta-2 microglobulin (B2M) (62.5%) levels, as well as aberrant cytogenetic abnormalities (16.7%). The cases were grouped into Stage III (39.7%), Stage II (24.4%), and Stage I (5.1%). CD38 and CD138 demonstrated 100% expression, with every case exhibiting expression of more than one aberrant antigen, including CD19 (28.2%), CD45 (23.1%), CD56 (83.3%), CD117 (25.6%), kappa (60.3%), and lambda light chain (38.5%). However, only CD19 markers and serum creatinine levels exhibited a statistically significant association (p = 0.036).
Conclusion: Immunophenotyping by multiparametric flow cytometry is powerful in distinguishing PCM from normal cells. The aberrant antigens expressed in this study displayed a heterogeneous immunophenotypic profile unique to our population. However, to enhance outcome and robustness of this study, it is recommended to engage additional centers purposefully to increase the sample size.
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
