Impact of Anthropometric and Genetic Factors on Plasma SIRT1 Level in Men with Essential Hypertension and Heart Failure
DOI:
https://doi.org/10.15419/bmrat.v11i4.875Keywords:
essential hypertension, heart failure, obesity, SIRT1 gene (rs7069102), sirtuin 1Abstract
Introduction: Sirtuin 1 (SIRT1) emerges as a promising biomarker for heart remodeling in the context of essential arterial hypertension (EAH). Additionally, the levels of certain plasma peptides might signal myocardial fibrosis and the progression of heart failure (HF) in hypertensive patients. Despite this potential, conflicting data exist regarding the marker's diagnostic value in HF patients. This study aims to explore the impact of anthropometric factors on plasma SIRT1 levels in men diagnosed with EAH and HF, considering the rs7069102 single nucleotide polymorphism (SNP) in the SIRT1 gene.
Methods: The study included an examination of 190 Ukrainian men aged between 40 and 65. The participants were divided into two groups: a control group, consisting of 70 individuals without cardiovascular disease (CVD), and a study group comprising 120 men with EAH, 60 of whom displayed signs of HF. Plasma SIRT1 levels were quantified using an enzyme-linked immunosorbent assay (ELISA), while the rs7069102 C/G polymorphism in the SIRT1 gene was detected through allele-specific polymerase chain reaction (PCR). The research employed various statistical methods, including correlation analysis, T-test, Mann-Whitney U test, one-way ANOVA, and analysis of contingency tables for data analysis.
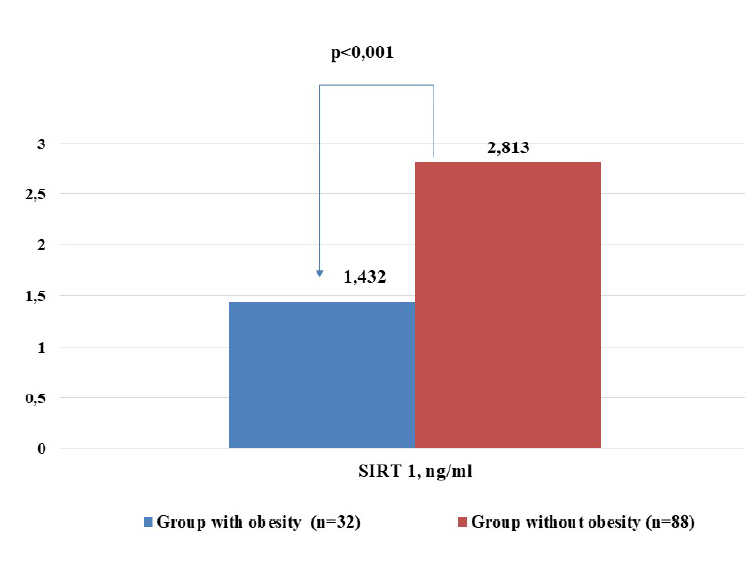
Results: The investigation revealed that men suffering from EAH and HF exhibited significantly reduced plasma SIRT1 levels (1.550 ± 0.084 ng/ml) compared to those with EAH but without HF (3.271 ± 0.238 ng/ml, p < 0.001). Notably, hypertensive men with concurrent HF and obesity or those with an early onset of hypertension showed even lower plasma SIRT1 concentrations. Interestingly, the analysis found no significant difference in plasma SIRT1 levels among individuals in the control group and EAH patients without HF across different rs7069102 C/G SNP variants. However, among hypertensive men with HF, individuals with the GG genotype displayed considerably lower plasma peptide levels compared to those with either the CC or CG genotype (1.390 ± 0.092 ng/ml vs. 1.744 ± 0.126 ng/ml, p = 0.032).
Conclusion: This study highlights a significant association between reduced plasma SIRT1 levels and heart failure in male patients with EAH. Factors contributing to decreased plasma peptide levels include obesity, early onset of hypertension, and possessing the GG variant of the rs7069102 SNP in the SIRT1 gene. These findings underscore the potential of SIRT1 as a marker for HF and may guide future therapeutic strategies.
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
