Utility of plasma galectin-3 in predicting long-term mortality in patients with acute heart failure
DOI:
https://doi.org/10.15419/bmrat.v8i4.669Keywords:
Galectin-3, Biomarkers, Prognosis, Acute Heart Failure, MortalityAbstract
Background: Several studies have investigated Galectin-3 as a promising biomarker for predicting the short-term and long-term mortality of patients with acute heart failure. This study aimed to examine the usefulness of plasma galectin-3 at the time of admission in predicting long-term mortality in Vietnamese patients with acute heart failure (AHF).
Methods: We carried out a cohort study including 117 patients consecutively diagnosed with acute heart failure in a single cardiology department. Plasma galectin-3 and other biomarkers were measured at the time of admission. The patient’s clinical and analytical characteristics were recorded. The main endpoint was one-year all-cause mortality.
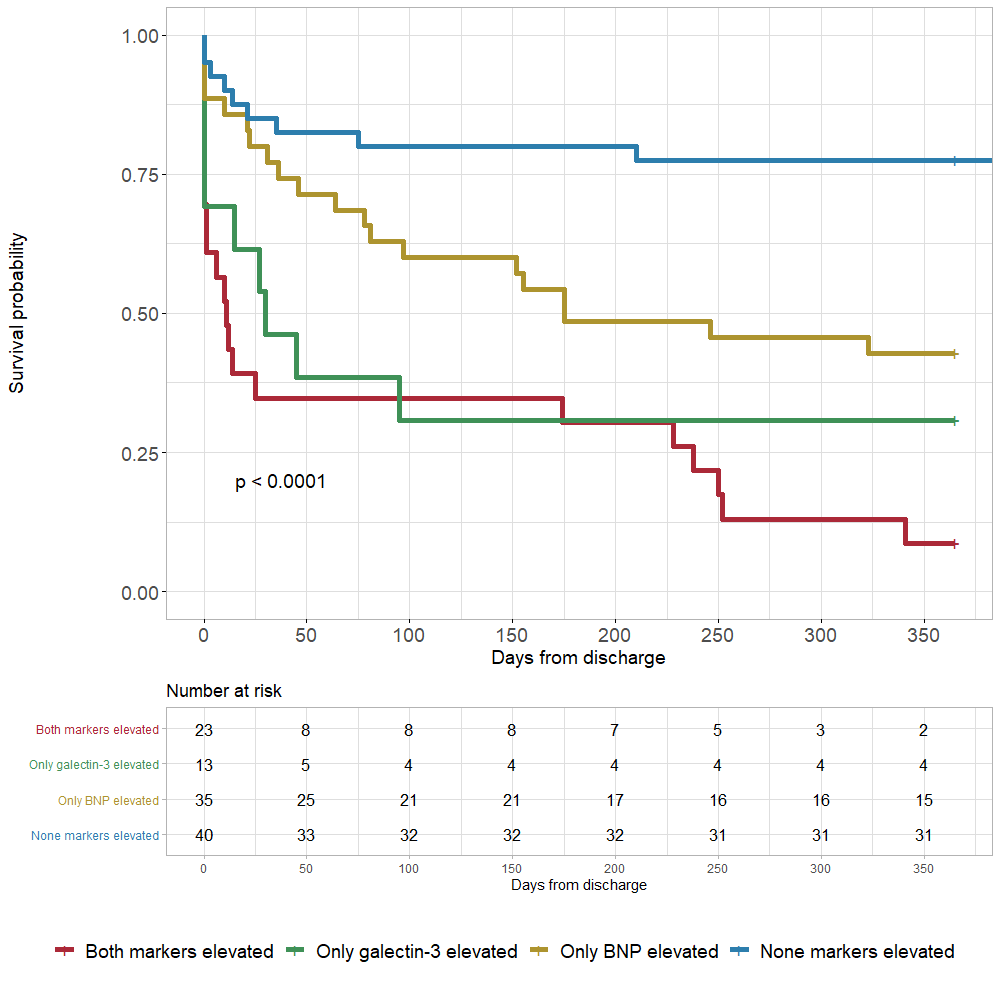
Results: There were six patients (5%) lost to follow-up and 59 patients (53.2%) reaching primary outcome within one year after hospital admission. The median plasma galectin-3 level (ng/mL) in patients with acute heart failure was 34.6 (26.7 – 44.1). Plasma galectin-3 in the alive group was significantly higher than that in the deceased group at one-year follow-up. In predicting one-year all-cause mortality, galectin-3 had an area under the curve (AUC) of 0.71 (95% confidence interval (CI), 0.62 – 0.81), representing a good prognostic factor, while brain natriuretic peptide (BNP) and troponin I were inferior to galectin-3 with an AUC of 0.69 (95% CI, 0.59 – 0.79) and 0.63 (95% CI, 0.53 – 0.74), respectively. The optimal cut-off value for galectin-3 was 40.75 ng/mL with a sensitivity of 50.1% and a specificity of 88.5%. In a multivariate model, patients with galectin-3 levels > 40.75 ng/mL had a hazard ratio (HR) of 2.8 (95% CI, 1.5 – 5; p = 0.001). The best prediction model was the combined model of galectin-3 and BNP, yielding an AUC of 0.78 (95% CI, 0.70 – 0.86; p < 0.001).
Conclusions: Our study suggested that galectin-3 levels could predict long-term all-cause mortality in patients with acute heart failure with a good prognostic capacity. Combining galectin-3 and BNP could yield better risk stratification.
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
