Autologous Bone Marrow Stem Cells combined with Allograft Cancellous Bone in Treatment of Nonunion
Abstract
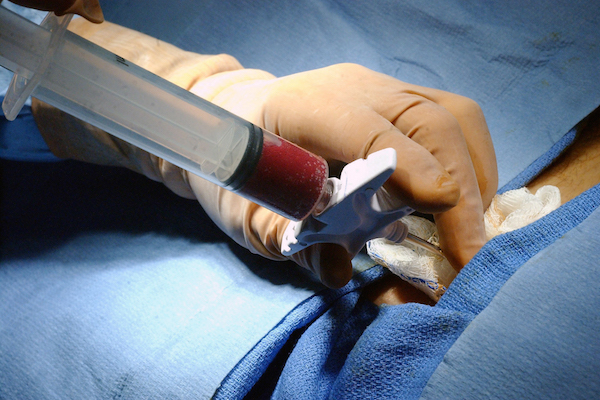
Autologous cancellous bone graft is currently used as a gold standard method for treatment of bone nonunion. However, there is a limit to the amount of autologous cancellous bone that can be harvested and the donor site morbidity presents a major disadvantage to autologous bone grafting. Embedding viable cells within biological scaffolds appears to be extremely promising. The purpose of this study was to assess the outcome of autologous bone marrow stem cells combined with a cancellous bone allograft as compared to an autologous bone graft in the treatment of bone nonunion. Bone marrow aspiration concentrate (BMAC) was previously produced from bone marrow aspirate via a density gradient centrifugation. Autologous cancellous bone was harvested in 9 patients and applied to the nonunion site. In 18 patients of the clinical trial group after the debridement, the bone gaps were filled with a composite of BMAC and allograft cancellous bone chips (BMAC-ACB). Bone consolidation was obtained in 88.9 %, and the mean interval between the cell transplantation and union was 4.6 ± 1.5 months in the autograft group. Bone union rate was 94.4 % in group of composite BMAC-ACB implantation. The time to union in BMAC-ACB grafting group was 3.3 ± 0.90 months, and led to faster healing when compared to the autograft. A mean concentration of autologous progenitor cells was found to be 2.43 ± 1.03 (x106) CD34+ cells/ml, and a mean viability of CD34+ cells was 97.97 ± 1.47 (%). This study shows that the implantation of BMAC has presented the efficacy for treatment of nonunion and may contribute an available alternative to autologous cancellous bone graft. But large clinical application of BM-MSCs requires a more appropriate and profound scientific investigations.
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
