Plasmablastic transformation of multiple myeloma post-autologous hematopoietic stem cell transplant
DOI:
https://doi.org/10.15419/bmrat.v10i8.820Keywords:
Plasmablastic Transformation, Plasmablastic Myeloma, Mutliple Myeloma, Post Autologous Haematopoietic Stem Cell TransplantAbstract
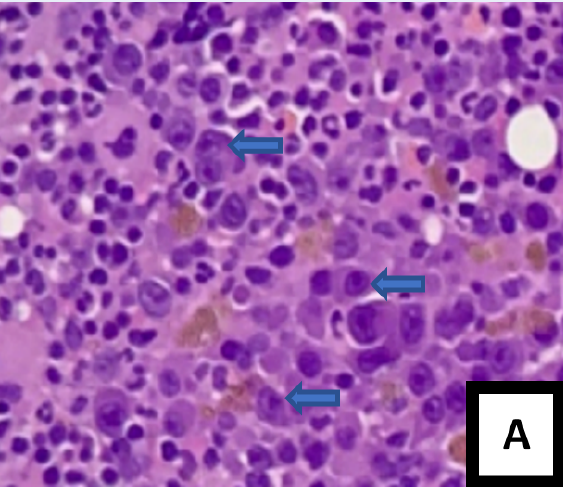
The present case report describes the uncommon and adverse plasmablastic transformation of multiple myeloma (MM) following autologous hematopoietic stem cell transplantation. To the best of our knowledge, this is the first case of plasmablastic myeloma (PBM) after an autologous hematopoietic transplant to be reported in Malaysia. A 41-year-old man initially diagnosed with MM IgG kappa reported lower back pain symptoms for a year, along with other associated symptoms. After receiving several lines of chemotherapy, the patient displayed a partial response (PR), and an autologous stem cell transplant (ASCT) was subsequently performed. Two months after the transplant, the patient showed signs of anemia, with a hemoglobin level of 8.0 g/dL. A peripheral blood film revealed the presence of a leucoerythroblastic blood film with normocytic normochromic red blood cells and rouleaux formation but no apparent plasma cells. The main infiltrating cells in the bone marrow aspirate (BMA) and trephine biopsy were plasmablasts with kappa light chain restriction. An increase in serum kappa free light chain (FLC), serum lambda FLC, and a low albumin/globulin (A/G) ratio were observed. In addition, serum protein electrophoresis showed an IgG kappa paraprotein band in the gamma region. Post-ASCT, the disease transformed into PBM, which conferred a poor prognosis on thepatient despite his post-transplant status. This case report highlights the diagnostic challenges of plasmablastic transformation in MM. Diagnosing PBM is thus crucial for the prompt and proper management of affected patients. Another consideration in the present case is whether the transplant procedure itself or the immunopathogenesis that took place after the ASCT resulted in the subsequent transformation into PBM.
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
