Comparison of the predictive value of prooxidant-antioxidant balance and heat shock proteins in the diagnosis of neonatal asphyxia
DOI:
https://doi.org/10.15419/bmrat.v4i05.171Keywords:
Asphyxia, Heat shock proteins (HSPs), Neonate, Prooxidant-Antioxidant Balance (PAB)Abstract
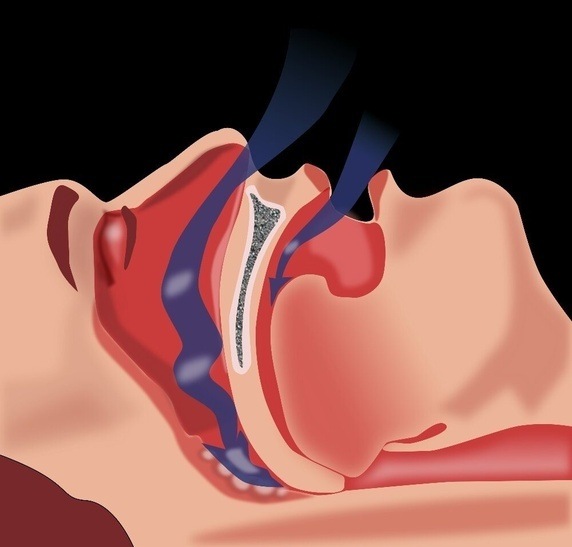
Introduction: Asphyxia is one of the important cause of infants' mortality. Accurate and early diagnosis of asphyxia has an important role in performing appropriate protective treatment protocole; therefore, we compared the diagnostic value of two methods of Prooxidant-Antioxidant Balance (PAB) and Heat shock proteins 70 ( HSP70) among healthy term infants and Neonates with asphyxia.
Methods: In this prospective case-control study, we compared the diagnostic value of two methods of PAB and HSP70 in healthy term infants (N=38) and Neonates with asphyxia (N=30) in Mashhad Ghaem hospital from 2011 to 2015. The diagnostic value of HSP70 and PAB was compared with statistical tests of Chi-square, T-Test, Man-Whitney, Roc curve and regression models.
Results: The newborns in two groups were significantly different in terms of the first (P=0.000) and fifth minute Apgar score (P=0.000), HSP70 (P=0.000), PAB (P=0.000), PH (P=0.000), BE (P=0.000) and HCO3 (P=0.015). HSP>0.218 ng / dl has 60% sensitivity and 76% specificity for the diagnosis of asphyxia while PAB>11.3 HK has 84% sensitivity and 92% specificity for the diagnosis of asphyxia.
Conclusion: According to the results of this study, HSP70>0.22 ng/dl and PAB>11.3 HK Unite can be used as biochemical markers for the diagnosis of perinatal asphyxia (P=0.001). The sensitivity and specificity of PAB in the diagnosis of asphyxia is higher than HSP70 and Simultaneous measurement of these two markers can correctly diagnose 84% of asphyxia cases.
References
Aly, H., Hassanein, S., Nada, A., Mohamed, M.H., Atef, S.H., and Atiea, W. (2009). Vascular endothelial growth factor in neonates with perinatal asphyxia. Brain and Development 31, 600-604.
Ashrafganjuee Umbilical cord entanglement and intrapartum complications during childbirth [Article in Persian]. J Shahrekord Univ Med Sci 2004, 2.
Ashrafganjuee (2004). Umbilical cord entanglement and intrapartum complications during childbirth [Article in Persian]. J Shahrekord Univ Med Sci, 2.
Bahman Bijari, B., Farahmandinia, Z., and Hazeghi, A. (2010). Predictive Value of Nucleated Red Blood Cell Counts in Cord and Peripheral Blood of Asphyxiated Term Neonates in the First Week of Life. SSU_Journals 17, 330-336.
Banupriya, C., Doureradjou, P., Mondal, N., Vishnu, B., and Koner, B. (2008). Can urinary excretion rate of malondialdehyde, uric acid and protein predict the severity and impending death in perinatal asphyxia? Clinical biochemistry 41, 968-973.
Basu, P., Som, S., Choudhuri, N., and Das, H. (2008). Correlation between Apgar score and urinary uric acid to creatinine ratio in perinatal asphyxia. Indian journal of clinical biochemistry 23, 361-364.
Boskabadi, H., Boroujeni, A.N., Mostafavi-Toroghi, H., Hosseini, G., Ghayour-Mobarhan, M., Alamdari, D.H., Biranvandi, M., Saber, H., and Ferns, G.A. (2014). Prooxidant-antioxidant balance in perinatal asphyxia. The Indian Journal of Pediatrics 81, 248-253.
Boskabadi, H., Maamouri, G., Sadeghian, M.H., Ghayour-Mobarhan, M., and Heidarzade, M. (2010). Early diagnosis of perinatal asphyxia by nucleated red blood cell count: a case-control study. Archives of Iranian medicine 13, 275.
Boskabadi, H., Omidian, M., Tavallai, S., Mohammadi, S., Parizadeh, M., Mobarhan, M.G., and Ferns, G.A. (2015). Serum Hsp70 antigen: Early diagnosis marker in perinatal asphyxia. Iranian journal of pediatrics 25.
Boskabadi H., P.Z., Barati T., Moedi A. (2010). Predisposing factors to investigate the causes of infant mortality in the city of Mashhad Ghaem hospital [Article in Persian]. Iran J Obstet Gynecol infertile 14, 6-14.
Ceccon, M.E.J.R. (2003). Interleukins in hypoxic-ischemic encephalopathy. Jornal de pediatria 79, 280-281.
Chen, H., Liu, Z., Zhou, Z., Jiang, M., Qian, L., and Wu, S. (2003). The regulatory effect of memantine on expression and synthesis of heat shock protein 70 gene in neonatal rat models with cerebral hypoxic ischemia. CHINESE MEDICAL JOURNAL-BEIJING-ENGLISH EDITION- 116, 558-564.
Chen, H.-J., Yau, K.-I.T., and Tsai, K.-S. (2000). Urinary uric acid/creatinine ratio as an additional marker of perinatal asphyxia. JOURNAL-FORMOSAN MEDICAL ASSOCIATION 99, 771-774.
Cheng, Y., Gidday, J.M., Yan, Q., Shah, A.R., and Holtzman, D.M. (1997). Marked age‐dependent neuroprotection by brain‐derived neurotrophic factor against neonatal hypoxic—ischemic brain injury. Annals of neurology 41, 521-529.
Cheng, Y., Liu, G., Guan, J., Guo, Y., Li, Y., and Wu, R. (2005). Early diffusion weighted imaging and expression of heat shock protein 70 in newborn pigs with hypoxic ischaemic encephalopathy. Postgraduate medical journal 81, 589-593.
Child, D.F., Hudson, P.R., Hunter-Lavin, C., Mukhergee, S., China, S., Williams, C.P., and Williams, J.H. (2006). Birth defects and anti–heat shock protein 70 antibodies in early pregnancy. Cell stress & chaperones 11, 101-105.
Fiedorowicz, M., Makarewicz, D., Stańczak-Mrozek, K.I., and Grieb, P. (2008). CDP-choline (citicoline) attenuates brain damage in a rat model of birth asphyxia. Acta Neurobiol Exp 68, 389-397.
Ghosh, B., Mittal, S., Kumar, S., and Dadhwal, V. (2003). Prediction of perinatal asphyxia with nucleated red blood cells in cord blood of newborns. International Journal of Gynecology & Obstetrics 81, 267-271.
Gunn, A.J., Gluckman, P.D., Wyatt, J.S., Thoresen, M., Edwards, A.D., and Group, C.S. (2005). Selective head cooling after neonatal encephalopathy. The Lancet 365, 1619-1620.
Hogan, L., Ingemarsson, I., Thorngren-Jerneck, K., and Herbst, A. (2007). How often is a low 5-min Apgar score in term newborns due to asphyxia? European Journal of Obstetrics & Gynecology and Reproductive Biology 130, 169-175.
Jiang, K., Yang, C., Shui, Q., Xia, Z., and Zhang, Y. (2004). Time-course of mu-calpain activation, c-Fos, c-Jun, HSP70 and HSP27 expression in hypoxic-ischemic neonatal rat brain. Zhonghua er ke za zhi= Chinese journal of pediatrics 42, 441-445.
Kliegman (2011). Hypoxia-ischemia. In Nelson textbook of Pediatrics 19th ed, K.M. Behrman ER, Arvin AM, eds., ed. (Philadelphia: WB Saundres Company), pp. 493-496.
Kumar, A., Ramakrishna, S.V.K., Basu, S., and Rao, G.R.K. (2008). Oxidative stress in perinatal asphyxia. Pediatric neurology 38, 181-185.
Lopriore, E., van Burk, G.F., Walther, F.J., and de Beaufort, A.J. (2004). Correct use of the Apgar score for resuscitated and intubated newborn babies: questionnaire study. Bmj 329, 143-144.
Low, J.A. (1997). Intrapartum fetal asphyxia: definition, diagnosis, and classification. American journal of obstetrics and gynecology 176, 957-959.
Marlow (2012). Do we need an apgar score? Arch Dis child 67, 765-767.
Menkes H., S.H. (2006). Perinatal asphyxia and trauma. In Child Neurology (MD:Williams and Wilkins: Philadelphia).
Ozer, E., Yilmaz, O., Akhisaroglu, M., Tuna, B., Bakiler, A., and Ozer, E. (2002). Heat shock protein 70 expression in neonatal rats after hypoxic stress. The Journal of Maternal-Fetal & Neonatal Medicine 12, 112-117.
Perlman, J.M. (1999). Markers of asphyxia and neonatal brain injury (Mass Medical Soc).
Rudiger (2008). Trial to Evaluate a Specified Type of APGAR.
Siciarz, A., Weinberger, B., Witz, G., Hiatt, M., and Hegyi, T. (2001). Urinary Thiobarbituric Acid–Reacting Substances as Potential Biomarkers of Intrauterine Hypoxia. Archives of pediatrics & adolescent medicine 155, 718-722.
Surai, P.F. (2007). Natural antioxidants in poultry nutrition: new developments. Paper presented at: Proceedings of the 16th European symposium on poultry nutrition (World Poultry Science Association).
Volpe, J. (1995). Neurology of the newborn 3rd ed. WB Saunders, Philadelphia.
Waldemar (2011). Nelson textbook of pediatrics (Philadelphia: Saunders).
Downloads
Published
Issue
Section
License
Copyright The Author(s) 2017. This article is published with open access by BioMedPress. This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
